-
PDF
- Split View
-
Views
-
Cite
Cite
Guray Togral, Murat Arıkan, Safak Gungor, Rare skeletal muscle metastasis after radical nephrectomy for renal cell carcinoma: evaluation of two cases, Journal of Surgical Case Reports, Volume 2014, Issue 10, October 2014, rju101, https://doi.org/10.1093/jscr/rju101
Close - Share Icon Share
Abstract
Renal cell carcinomas (RCCs) commonly cause metastases to the lung, liver, bone and brain but rarely to the skeletal muscles. We describe solitary large masses located in the gluteus maximus and medius muscles in two patients who had a history of RCC treated with nephrectomy. Metastatic RCC must be distinguished from benign primary soft tissue tumors because it requires aggressive surgical resection. An open incisional biopsy revealed RCC metastasis. Both patients underwent complete resection of the large mass with additional local radiotherapy and immunochemotherapy. This incalculable course of RCC suggests the need to perform a thorough postoperative follow-up of such patients.
INTRODUCTION
Renal cell carcinoma (RCC) accounts for 3% of adult solid tumors. RCC is detected in patients aged 50–70 years. The most common sites of RCC metastases are the lung (50%), lymph nodes (35%), liver (30%), bone (30%), adrenal glands (5%) and brain [1]. The skeletal muscle is a rare site of metastasis, accounting for <1% of metastases. Skeletal muscle metastasis is detected at presentation or develops during the follow-up period after radical nephrectomy for RCC (∼0.4%) [2]. From a recent review of the English literature, only 35 cases of skeletal muscle metastasis of RCC have been reported [3]. Diagnosis of metastatic RCC to the skeletal muscle is challenging, as the site is unpredictable. Furthermore, cases of metastasis arising long after nephrectomy have been reported. One-third of patients with RCC have metastatic disease, and surgery is a major component of the treatment. In the absence of distant metastases, nephrectomy is an accepted curative treatment. We describe two cases with an unusual presentation of skeletal large muscle metastases of RCC and emphasize the importance of annual surveillance for metastatic RCC even after curative nephrectomy.
CASE REPORT
Case 1
A 67-year-old man was admitted to our orthopedic clinic for a painful hard mass that had been slowly growing for >1 year at the posterolateral aspect of the right thigh. He had a 9-year history of left radical nephrectomy for a 6-cm diameter RCC (stage II [pT1 N0 Mx], nuclear grade Fuhrman grade III/IV). On physical examination, a 10 × 7 cm palpable mass was detected at the right posterolateral gluteal region. Magnetic resonance imaging (MRI) revealed a 165 × 75 × 67 cm hypervascular lesion within the gluteus maximus muscle, with unclear borders to the biceps femoris (Fig. 1A and B). After an incisional biopsy, the mass was reported as an RCC metastasis (Fig. 2A and B). Total excision of the mass was performed. Histochemical analysis of the total excision specimen revealed positive staining for cytokeratin, RCC and vimentin confirming the diagnosis. We performed a total body bone scan (Fig. 1C) to achieve complete stadiation of the mass. After complete healing, external radiotherapy was administered at 30 Gy to the right leg, in the surgical site, with an additional three cycles of immunotherapy regimen, including interferon-α (IFN-α), interleukin 2 and sunitinib therapy.
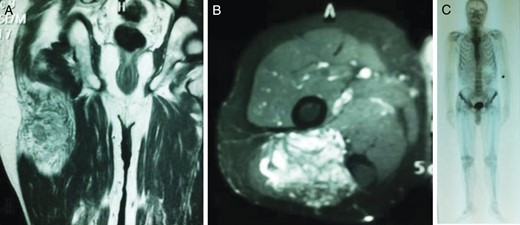
Coronal (A) and axial (B) T2-weighted fat-suppressed images showing the encapsulated soft tissue mass within the right gluteus maximus muscle; (C) whole-body bone scintigraphic image.
![(A) Histopathologic appearance of the RCC metastasis in the right gluteus maximus muscle (hematoxylin-eosin [H&E] staining, original magnification ×100) and (B) histochemical assay result of the fine-needle biopsy of the mass positive for RCC (RCC ×200).](https://oupdevcdn.silverchair-staging.com/oup/backfile/Content_public/Journal/jscr/2014/10/10.1093_jscr_rju101/2/m_rju10102.jpeg?Expires=1773164657&Signature=NJb96JX1oWzZUIFjUIXnSrYBPSWTzQDRheNyTWzgVf~I~IfhvcHzNjTVl-qQrJGnoivJd8xoTYi1sCr2WB4Jdf48X4sETNP7IOy2YmEy7AaSt3CiRhFvoNYpKkqt-KmsR-A9HzRyiAd9LB4WKPBlHaCrgjv1EhfNFs2eDBTsRzQ6p26OpTxq9tJA~T9IuMb5G6lwSdwdStkRUrxaphZyF3mfYHWC46gUVc2LuzliUh9A1lFVdqglSnMB4omR2k~qGPGPTEgEx1pfut9CAPBSGrxCz0NLenISTjfKzzatl5nUOHENx45OGeTmCMkLyxZv9R-YqCpkWFmGmdnGz0F-4g__&Key-Pair-Id=APKAIYYTVHKX7JZB5EAA)
(A) Histopathologic appearance of the RCC metastasis in the right gluteus maximus muscle (hematoxylin-eosin [H&E] staining, original magnification ×100) and (B) histochemical assay result of the fine-needle biopsy of the mass positive for RCC (RCC ×200).
Case 2
A 74-year-old man presented to the orthopedics outpatient clinic with painless swelling on his right leg that had developed progressively in the last 3 months. He underwent right radical nephrectomy for RCC 7 months prior. A pathological examination of the right kidney demonstrated the presence of clear cell carcinoma and Fuhrman grade IV (pT2 N0 Mx). On physical examination, an 8 × 6 cm hard mass was palpable on the lateral aspect of his right leg. MRI of his right leg revealed a 10 × 8.5 × 5.5 cm tumor located in the gluteus medius muscle (Fig. 3A and B). Computed tomography, ultrasonography and MRI did not reveal any liver or retroperitoneal lymph node metastasis. A total body bone scan of the patient showed no abnormalities (Fig. 3C). Biopsy of the muscle mass documented an RCC metastasis (Fig. 4A and B). The mass was completely removed from the right leg. The patient underwent three cycles of immunotherapy regimen, including IFN-α.
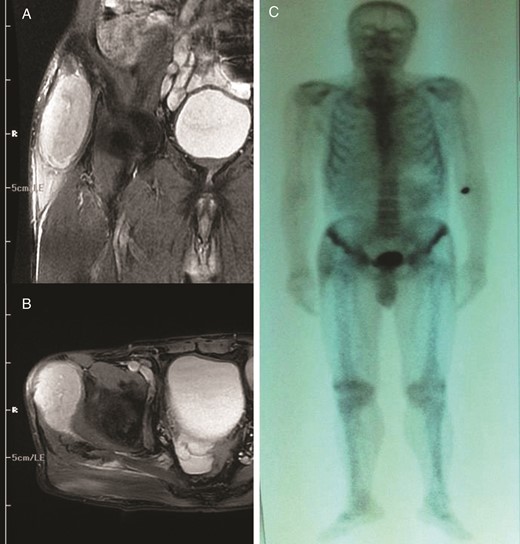
Coronal (A) and axial (B) T2-weighted axial magnetic resonance image of the right gluteus medius muscle showing avid enhancement of the soft tissue component. (C) Total body bone scan image.
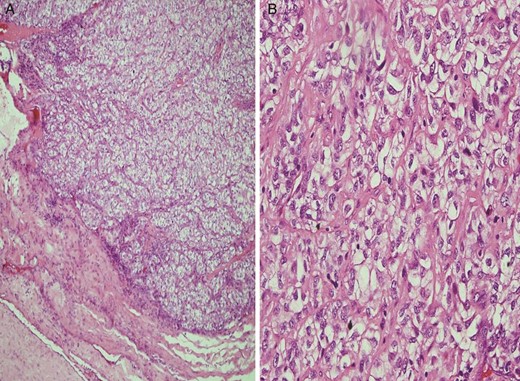
(A) Light microscopic image showing malignant cells with clear cytoplasm invading the surrounding soft tissue and skeletal muscle (H&E staining, original magnification ×100) (A) and (B) light microscopic image (H&E staining, original magnification ×400) showing malignant cells with clear cytoplasm and pleomorphic vesicular nuclei.
DISCUSSION
Atypical presentations and distant metastasis are characteristic of RCC. RCC rarely spreads to the skeletal muscle, with a reported percentage of only 0.4% [4]. Despite its rich blood supply and large surface area, the skeletal muscle is a rare site of metastasis. The mechanism involved in metastasis to the skeletal muscular tissue is not well understood. However, the presence of protease inhibitors in the basement membrane inhibiting cell invasion, increased lactic acid levels and acidic environment interfering with tumor cell growth were described as possible causes [5]. A solitary soft tissue mass develops any time between 6 months and 19 years, with the greatest risk in the first 5 years after initial presentation [4]. The location, size and absence of pain in our patients were indicative of soft tissue sarcoma. However, detection of metastases to the skeletal muscle is difficult because of the painless nature of the tumors and their small size [6]. It was reported that in 11% of cases, metastatic RCC occurred >10 years after initial diagnosis [7]. In a series of 121 patients with soft tissue metastasis, the most common primary source was lung cancer (31%), followed by renal carcinoma (12%) and colon cancer (8%) metastasizing to soft tissues [8]. These organ systems might be possible primary tumor sources in a patient with soft tissue metastasis. RCC is known to metastasize to soft tissues nearly always as a solitary soft tissue deposit, developing from a few months to several years after the initial diagnosis of RCC. Metastatic RCC to the skeletal muscle must be differentiated from primary soft tissue tumors because primary soft tissue tumors are more common than metastatic tumors to the skeletal muscle. A biopsy should be performed. We prefer open biopsy for hypervascular soft tissue masses to avoid this catastrophic complication. MRI is the most important imaging technique for differentiation of soft tissue metastases from primary sarcomas and other pathologies. Angiographic examinations show that metastatic RCC to the skeletal muscle usually appears as hypervascular lesions [6]. However, in our two cases, the patients were unusually diagnosed initially with skeletal muscle metastasis of RCC and had undergone radical nephrectomy for RCC. Nephrectomy and excision are currently the treatments of choice for solitary metastatic lesions, with a reported 5-year survival rate of 20–30% [9]. Therefore, we believe that annual computed tomography examinations of the lung and abdomen should be performed during the first 10 years after radical nephrectomy in patients with an RCC greater than stage pT2. Kwak et al. [10] reported that metastasectomy status was an absolute factor of overall survival in patients with metastatic RCC.
We recommend continuing intensive follow-up examinations for RCC metastasis, especially for high-grade tumors, even after 10 years of initial tumor presentation or long disease-free interval.



