-
PDF
- Split View
-
Views
-
Cite
Cite
Sankar Narayanan ML, C. D. Narayanan, Anupma J. Kindo, Apurva Arora, Priya A. Haridas, Fatal fungal infection: the living dead, Journal of Surgical Case Reports, Volume 2014, Issue 10, October 2014, rju104, https://doi.org/10.1093/jscr/rju104
Close - Share Icon Share
Abstract
Necrotizing fasciitis is an uncommon infection mainly caused by Streptococcus pyogenes, which is also known as flesh-eating bacteria. It is often caused by bacteria, but can also be caused and complicated by fungus. We report a case of bacterial necrotizing fasciitis that was complicated by a fatal fungal infection, a rare clinical presentation affecting the upper limbs, head and neck, in a young diabetic female patient. It was an unsuspected case of fungal infection with mucormycosis, which proved to be fatal due to a delay in diagnosis and treatment.
INTRODUCTION
Primary cutaneous zygomycosis leading to necrotizing fasciitis is a rare complication in diabetic patients. Necrotizing fasciitis is characterized by rapidly progressive necrosis of skin, subcutaneous tissue and superficial fascia. These are mainly bacterial in origin and are associated with severe sepsis and mortality [1]. Infections by fungi of the zygomycetes group may be responsible for fatal necrotizing infection in diabetic patients, as will be seen in the present case.
CASE REPORT
A 30-year-old lady presented in the emergency room with swelling and pain of the right shoulder for the previous 4 days. She reported a minor trauma to her right shoulder a week previously, following which she developed swelling and pain, associated with high-grade fever. She was a known diabetic and had been receiving treatment with oral hypoglycaemic agents for the last 5 years.
On clinical examination, the patient was toxic, febrile, tachypnoeic and had tachycardia. On local examination there was a diffuse swelling involving the right shoulder, neck and anterior chest wall, and the overlying skin was inflamed. There was local rise in temperature with tenderness and marked induration. There was gross oedema involving the face and the patient had difficulty in breathing.
Contrast-enhanced computed tomography (CT) scan showed extensive cellulitis and thrombosis of the internal jugular vein and marked necrosis of the underlying muscles (Figs 1 and 2). The basic investigations revealed a haemoglobin level of 7.5 g/dl, a random plasma glucose level of 227 mg/dl and the fasting glucose level was 240 mg/dl.

Contrast-enhanced CT. At level of the mediastinum shows extensive inflammation involving the fat and the muscles on the right side.
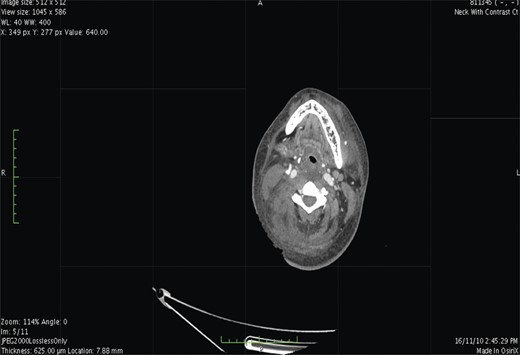
Contrast-enhanced CT. At the level of base of skull shows airway luminal narrowing.
The total count was elevated to 16 370 mm3 and arterial blood gas showed metabolic acidosis.
The patient was started on intravenous piperacillin tazobactam and was subsequently taken for emergency debridement of the wound on the right shoulder. During surgery, as the wound was being debrided, there was practically no bleeding (Fig. 3). There was extensive necrosis involving the scapular, neck and facial muscles, although the subcutaneous tissue and the overlying skin looked apparently normal. The tissue was sent for histopathology and, to our surprise, it turned out to be positive for fungal elements. Examination showed acute on chronic inflammatory cell infiltrate, necrosis and splaying of muscle fibres. Many broad aseptate fungal elements morphologically resembling features of the zygomycetes group were seen (Fig. 4). Special staining on periodic acid Schiff (PAS) stain also showed clusters of broad aseptate fungal hyphae.

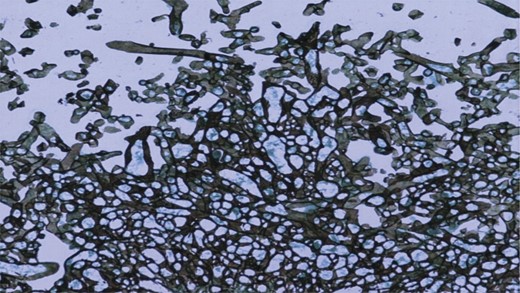
PAS stain showed clusters of broad aseptate fungal hyphae. (10× magnification).
Culture swab taken from the wound site isolated Klebsiella pneumoniae and Enterobacter cloacae, and the antibiotics were changed to imipenem and cilastatin. As the patient's condition had not improved, despite antibiotic treatment, she was taken for re-debridement under general anaesthetic. The entire dead tissue was removed until active bleeding was seen (Fig. 5) and tissue sent for histopathological examination.

The patient was started on amphotericin B after the histopathological report confirmed fungal Infection, but she succumbed to the infection after 2 days.
DISCUSSION
Necrotizing fasciitis is a common surgical problem often encountered as an emergency, wherein aggressive debridement usually saves the life of the patient. It is quiet common for a surgeon to encounter bacterial infection causing necrotizing fasciitis. Most bacteria and fungi that can multiply in the soft tissues are contained within the fascia.
Fungi of the class zygomycetes are distributed worldwide and are commonly found in the soil and in plant debris [2]. Infections with this class of fungi occur in patients who have a history of trauma with underlying conditions of immunosuppression [3]. The fungi are implanted at the site of trauma and cause cellulitis if not diagnosed immediately.
These are highly invasive organisms. They invade the blood vessels and proliferate, resulting in emboli formation and also damage the blood vessels leading to necrosis of the surrounding tissue [4].
Cutaneous necrotizing mucormycosis remains a medical challenge. Its rarity requires a broad suspicion and clinical diagnosis in order to salvage the patient. Its aggressive nature demands prompt surgical and anti-fungal intervention.
Fungi of different classes distributed worldwide are commonly found in plant debris and soil, but have also been isolated from food and indoor air. Fungal infection usually affects patients with underlying risk factors such as acidosis, hyperglycaemia, acute renal failure and those taking antibiotics for long periods.
After invading the human body through traumatized tissue, zygomycetes have an affinity for blood vessels and invade perivascular structure with their hyphae, resulting in vessel damage. This can also cause formation of emboli, infarcts and tissue necrosis.
Depending on the co-morbid conditions, the infection may vary from limb oedema to life-threatening sequelae. Many bacteria (group A-streptococci) can trigger multi system organ failure and septic shock. Depending on the location, there are descriptive terms, for example, Fournier's gangrene necrotizing perineal infection. Extensive necrosis with thrombosed vessels with subcutaneous and muscle involvement should make one think of fungus as a cause of infection, especially in immunocompromized individual.
Most necrotizing soft tissue infections are polymicrobial, hence broad-spectrum coverage is advisable. Options include combinations such as ampicillin, gentamycin, clindamycin or metronidazole and pipercillin tazobactam (Zosyn®), which provide adequate anaerobic and aerobic coverage.
Imipenem cilastatin provides extensive broad spectrum coverage. This combination agent is active against nosocomial Gram-negative bacilli, such as Enterobacter sp., Acinetobacter sp., Proteus vulgaris and P.aeruginosa. Because of this extensive coverage imipenem cilastatin B-lactamase inhibitors have been used successfully as single agents in the treatment of necrotizing soft tissue infections. In this patient, if there had been early diagnosis or even had there been clinical suspicion of fungal infection treatment using parental amphotericin with surgical debridement could have prevented progression of disease and prevented mortality. Another treatment option is use of hyperbaric oxygen therapy, as an adjunct to surgical debridement and not as a replacement.
Fungal cellulitis should always be kept in mind when treating diabetic patients with trauma or non-healing ulcers. It is almost impossible to save a patient past the point where the fungus has invaded the blood vessels and produced massive necrosis. Timely aggressive intervention is required to prevent mortality. It is now our current practice to send tissues debrided for fungal staining and culture in normal saline. Where hyphae are seen, patients are immediately started on antifungal therapy, even prior to the culture report in immunocompromized patients. We have seen good responses where patients improve dramatically after antifungal therapy.
Fungal stains and culture are routine in immunocompromized patients, wounds sustained following road traffic accidents and prolonged antibiotic therapy. With this new policy in place, we have achieved faster wound healing and lower mortality due to sepsis.



