-
PDF
- Split View
-
Views
-
Cite
Cite
Kotoe Kamata, Takashi Maruyama, Masayuki Nitta, Makoto Ozaki, Yoshihiro Muragaki, Yoshikazu Okada, A case of loss of consciousness with contralateral acute subdural haematoma during awake craniotomy, Journal of Surgical Case Reports, Volume 2014, Issue 10, October 2014, rju098, https://doi.org/10.1093/jscr/rju098
Close - Share Icon Share
Abstract
We are reporting the case of a 56-year-old woman who developed loss of consciousness during awake craniotomy. A thin subdural haematoma in the contralateral side of the craniotomy was identified with intraoperative magnetic resonance imaging and subsequently removed. Our case indicates that contralateral acute subdural haematoma could be a cause of deterioration of the conscious level during awake craniotomy.
INTRODUCTION
Awake craniotomy has contributed to expanding the surgical indication of especially tumours adjacent to the eloquent area. Concerns about patient management during awake craniotomy include: (i) keeping spontaneous respiration with an unsecured airway; (ii) potential risks of sudden onset nausea/vomiting and seizure; (iii) requirement of the multimodal approach to pain; and (iv) keeping the constant level of consciousness. Our surgical strategy for glioma resection showed good resection and survival rates compared with historical data [1]. From March 2000 to August 2013, we had experienced 1235 craniotomies with the use of intraoperative magnetic resonance imaging (iMRI), of which 1 000 cases were surgeries for intracranial glioma, and 300 of these cases were managed by awake surgeries. In this report, we present a case of loss of consciousness during awake craniotomy. Based on careful differential diagnosis, acute subdural haematoma (ASDH), which was incidentally found by iMRI, caused deterioration of the conscious level though haemorrhage did not extend like a typical traumatic brain injury case.
CASE REPORT
A 156 cm, 60 kg, 56-year-old woman complained of mild motor aphasia and right hemiparesis. MRI revealed a mass lesion with ring-like enhancement (45 × 42 × 48 mm) in the left frontal lobe with midline shift. Awake craniotomy with iMRI was scheduled because the tumour was located in the left superior and middle frontal gyri.
General anaesthesia was induced. Following left frontal craniotomy and dural incision, the first iMRI was performed (Fig. 1 ). One hundred fifty-eight minutes from induction, the patient regained consciousness after all anaesthetics were ceased. Tumour resection was performed with free conversation. However, after 143 min of surgery under the awake condition, the patient came to complain of excessive sleepiness though she could respond to verbal commands. Electrocorticogram (ECoG) did not detect after-discharge. The tumour was successfully removed en bloc fashion. Progressive brain swelling was not observed. The second iMRI was commenced 182 min into the awake phase (Fig. 2). Thirteen minutes from the beginning of the second iMRI scanning, the patient did not respond to noxious stimuli. When the patient was removed from the gantry, she was unconscious and had stopped spontaneous breathing. Her pupils were isocoria and did not dilate. Neither epileptic seizure nor anaphylactic reaction occurred. The peripheral oxygen saturation was not measurable, but cardiac instability or signs of vomiting were not observed. We decided to discontinue the operation under the awake status. No electrolyte imbalance or hypoglycaemia was observed. Subsequently performed iMRI identified a thin subdural haematoma in the contralateral side (Fig. 3). The fourth iMRI confirmed that most of the haematoma was evacuated following right frontal craniotomy.
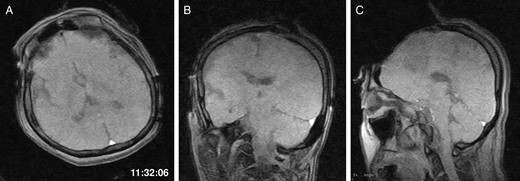
The first intraoperative magnetic resonance images performed after the craniotomy. (A) Axial, (B) coronal and (C) sagittal T1-weighted scout images show the left frontal tumour. The time of scan is superimposed.
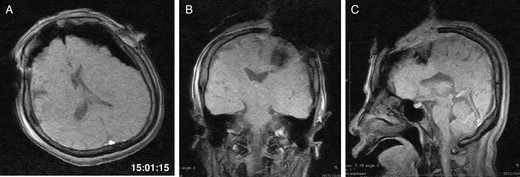
The second iMRI was performed after the tumour resection. (A) Axial, (B) coronal and (C) sagittal T1-weighted scout images show no intracranial haemorrhage. The time of scan is superimposed.
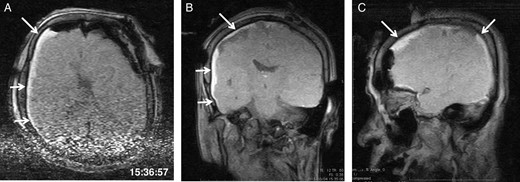
The third intraoperative magnetic resonance images after intubation, axial (A), coronal (B) and sagittal (C) T1-weighted scout images show acute right-sided subdural hematoma (arrows), contralateral to the site of the craniotomy. The time of scan is superimposed.
Postoperative computed tomography (CT) revealed neither intracranial haematoma nor pin-related fracture. The patient was extubated 90 min after the end of operation. Both blood pressure and coagulation parameters were kept within normal limits. She recovered without neurological deficits.
DISCUSSION
An important caution learned from this case is to expect contralateral hematoma as a cause of deterioration of the conscious level during awake craniotomy despite a haemorrhage not being as extensive as that caused by traumatic injury. Several factors are considered with patient decline during awake craniotomy, including subclinical epilepsy, cerebral infarction, cerebral haemorrhage, cerebral oedema, or psychogenic reaction called hysteria. In our patient, neither epileptiform activity nor after-discharge was recorded on ECoG. Both motor and sensory-evoked potentials were stable throughout the operation. Progressive brain swelling was not observed surgically. Psychogenic reaction did not occur though awake craniotomy is recognized as a significant psychological stressor [2]. She did not complain of pain or discomfort while awake. In fact, her postoperative psychological sequelae did not resemble posttraumatic stress disorder symptoms. Thus, contralateral subdural haematoma was suspected to be the main reason of our patient's decline.
The aetiology of remote intracerebral haemorrhage remains unclear. As Shen et al. [3] reported, the elderly population is more susceptible to contralateral ASDH than young patients and the average age of previously reported ASDH cases was 52 years. Brain atrophy with increasing subdural space is progressive with ageing. Therefore, mechanical brain shift and subdural space detachment from the cerebral parenchyma occurs opposite to craniectomy, causing damage to the bridging veins [3]. Additionally, looser adhesion between dura and skull inner table at both frontal and parietal lobes is considered to be one reason that subdural haemorrhages frequently occur at those areas [3]. In our case, surgical defect with brain shift was the only finding before the patient lost consciousness (Fig. 2). As subdural haemorrhages generally result from shearing injuries, it can be speculated that this brain shift owing to surgical intervention gradually damaged the bridging veins by reducing the volume of cerebral spinal fluid. Then, tumour removal had a decompressive impact that caused tearing of the stretched bridging veins and released a tamponade effect. Consequently, ASDH which was found immediately after tumour removal was thin, not extensive. This hypothesis of haematoma formation could also explain the time course of patient deterioration when she started to complain of excessive sleepiness as the tumour was removed. We should remind that ASDH affects patients' conscious level during awake craniotomy.
To our knowledge, this is the first reported case of ASDH diagnosed by iMRI. Haemorrhage is recognized as one of the major complications in neurosurgical patients [4]. Since the majority of the remote haemorrhages develop during or soon after surgery, postoperative routine CT study has been recommended [4]. Postoperative CT is a reliable way to evaluate potential complications when a patient rapidly recovers. However, in some cases, the patient may not survive because the CT unit is commonly located a long distance from the operating theatre. Tsermoulas and Mitchell described a case with a contralateral acute extradural haematoma detected by intraoperative ultrasound [5]. Of course, intraoperative ultrasound or MRI studies will not be an alternative to CT, but these cases indicate that intraoperative examinations contribute to early diagnosis of unexpected complications.
Contralateral ASDH is a rare but potentially lethal complication during awake craniotomy since ASDH causes deterioration of the conscious level. We should detect and rule out such contralateral haematoma formation to prevent patient decline.
ACKNOWLEDGEMENTS
The authors are indebted to Dr Naoko Saito (Department of Radiology, Saitama International Medical Centre, Saitama Medical University) for her expert advice. This clinical observation has never been published and is not currently being reviewed by any other publication medium. The authors report no conflict of interest concerning the materials, methods and the findings specified in this paper. The present report was supported solely by hospital and/or departmental resources. In addition, the authors have participated in the conception of this case report; and have all assisted in revising the case for important intellectual content.



