-
PDF
- Split View
-
Views
-
Cite
Cite
Rohit A. Singh, Krishnanand R. Pai, Chris M.R. Satur, Delayed presentation of an aspirated capsule endoscope, Journal of Surgical Case Reports, Volume 2013, Issue 9, September 2013, rjt082, https://doi.org/10.1093/jscr/rjt082
Close - Share Icon Share
Abstract
Capsule endoscopy has revolutionized the investigation of small intestinal pathology with an increasing repertoire of indications. We present the first reported case of an aspirated capsule presenting after a long asymptomatic period that was removed with no permanent pulmonary sequelae. This report highlights a cohort of patients who could be susceptible to this rare complication. The report also encourages the development of local/national guidelines to investigate misplaced/lost capsules during the procedure.
INTRODUCTION
Capsule endoscopy has revolutionized the investigation of small intestinal pathology with an increasing repertoire of indications. Aspiration of a capsule endoscope is an uncommon, but potentially hazardous complication. We present a case of delayed presentation of an aspirated capsule.
CASE REPORT
A 56-year-old gentleman presented with a 2-week history of progressive shortness of breath following a coughing fit whilst having a meal. He is a reformed smoker, with mild chronic airway disease, hypertension, gout and a left-sided cerebrovascular accident (CVA) in 2006 with complete neurological recovery. He had been investigated 6 weeks previously for iron deficiency anaemia with a capsule endoscopy, which was reportedly ‘lost’ during the procedure. An esophagogastroscopy performed immediately failed to locate the capsule. The patient refused any further investigations to locate the capsule.
Chest X-ray (Fig. 1) and computed tomography (CT) scan (Fig. 2) revealed a foreign body in the right bronchus intermedius with collapse and consolidation of the distal bronchial tree. The gentleman was transferred to the cardiothoracic unit. An adult Negus rigid bronchoscope introduced under general anaesthesia revealed a metallic foreign body with smooth rounded contours wedged in the bronchus intermedius. This was removed using a Wolfe lighted grabber. The foreign body was a capsule endoscope (Given Imaging Limited, Israel) (Fig. 3).
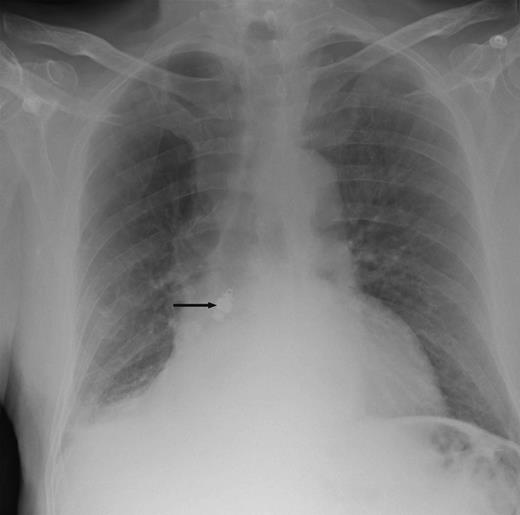
Chest X-ray showing a metallic foreign body impacted in the right bronchus with collapse of the middle and lower lobes on the right side.
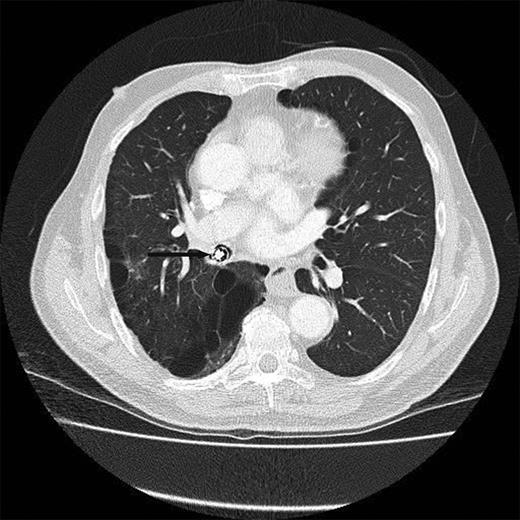
CT scan showing the metallic object in and completely obstructing the bronchus intermedius.

The patient received post-operative antibiotics and intensive physiotherapy. Chest X-ray prior to discharge revealed complete resolution of the atelectasis and consolidation. The patient continues to do well on follow-up. On retrospective questioning the patient denied any problems in swallowing the capsule endoscope.
DISCUSSION
Capsule endoscopy is a safe procedure with the main complication being retention of capsule in 0.75–2.0% cases [1]. Aspiration of the capsule is rare and reported in 11 cases in literature [2]. Most cases were diagnosed immediately based on symptoms of aspiration or images of the bronchial tree relayed by the capsule [3–5]. A common theme in these reports is the prevalence of an elderly cohort with a past history of CVA with/without the presence of swallowing abnormalities. The presence of obvious swallowing abnormalities is contraindication for conventional capsule endoscopy [6].
Interestingly, in this case, the patient was middle aged with fully recovered CVA and no obvious swallowing abnormality. There were no clinical symptoms to suggest aspiration of the capsule during the initial procedure. When the capsule was ‘lost’, an esophagogastroscopy performed immediately failed to reveal the capsule, while a chest X-ray might have shown the aspirated capsule. This is, also to our knowledge, the first reported case of an aspirated capsule presenting after a long asymptomatic period of almost 6 weeks after the initial procedure. This is not unusual as foreign bodies in the bronchus can have asymptomatic periods lasting weeks before presenting with complications [7]. The learning points we would like to highlight in this case report are the increased risk of aspiration in patients with a previous stroke even without an obvious swallowing abnormality and also encourage the development of local protocols to investigate ‘lost’ capsules, including the use of a chest roentgenogram to diagnose the rare occurrence of aspiration that could potentially present later with major pulmonary complications. This would improve the safety profile of this investigation.
In conclusion, we report a case of delayed presentation of an aspirated capsule endoscope, removed with no permanent pulmonary sequelae. This report highlights a cohort of patients who could be susceptible to this rare complication. The report also encourages the development of local/national guidelines to investigate misplaced/lost capsules during the procedure.



