-
PDF
- Split View
-
Views
-
Cite
Cite
Patrick Tomasetti, Philipp Metzler, Christine Jacobsen, Isolated inferior rectus muscle rupture after blunt orbital trauma, Journal of Surgical Case Reports, Volume 2013, Issue 9, September 2013, rjt076, https://doi.org/10.1093/jscr/rjt076
Close - Share Icon Share
Abstract
A 44-year-old man was referred to our department with diplopia, periorbital swelling and haematoma of the left eye after orbital trauma due to a punch. During the examination, mild enophthalmos, hypertropia and a total absence of infraduction were observed. An orbital computed tomography (CT) scan demonstrated a left orbital floor blow-out fracture, with caudal herniation of periorbital fat and rectus inferior muscle. Repair was performed under total anaesthesia with placement of a Titan mesh. The following days were marked by the persistence of diplopia without improvement of infraduction. A postoperative, 0.5 mm CT scan highlighted a complete rupture of the inferior rectus muscle, not seen before operation, by a 1.0 mm-sliced CT. In this case, orthoptic therapy was undertaken with good results after 6 months and without need of a second repair.
INTRODUCTION
Orbital fractures are common sequelae of blunt trauma to the periocular region. Diplopia after orbital-floor fracture is not rare and is commonly attributed to incarceration of an extraocular muscle in the fracture site. Palsy of a cranial nerve or its branch, or adhesion to scar tissues, are also reported to contribute to post-traumatic strabismus [1].
In cases of vertical diplopia, traumatic inferior rectus muscle (IR) rupture is a rare, but possible cause of persistent infraduction deficit after blow-out fracture that has to be taken into account. Few cases have been published in the literature [2]. We describe such an uncommon case with a review of the relevant published literature.
CASE REPORT
A 44-year-old man was referred to our department with a monocular hematoma, swelling and diplopia. He was punched in the area of the left orbit the day prior during a violent conflict.
The clinical examination revealed a left-side periorbital swelling and monocular hematoma with significant subconjunctival haemorrhage. A vertical diplopia with restriction of infraduction was also observed (Fig. 1). Additionally, he presented with hyperopia. The palpation of the underlying bone showed no bony step-off of the orbital rim. A preoperative ophthalmological evaluation confirmed the vertical diplopia, and showed an isolated IR muscle underaction with deficiency of depression in abduction, as well as a vertical deviation in primary position.

Preoperative clinical presentation in straight (left) and down gaze (right) view shows hyperopia and a restriction of infra-duction.
Computed tomography (CT 1 mm slices) presented a large, left-orbital floor fracture with caudal dislocation of the bone fragment and prolapse of the IR muscle and orbital fat into the maxillary sinus (Fig. 2a). Transection or disinsertion of the IR was not described.
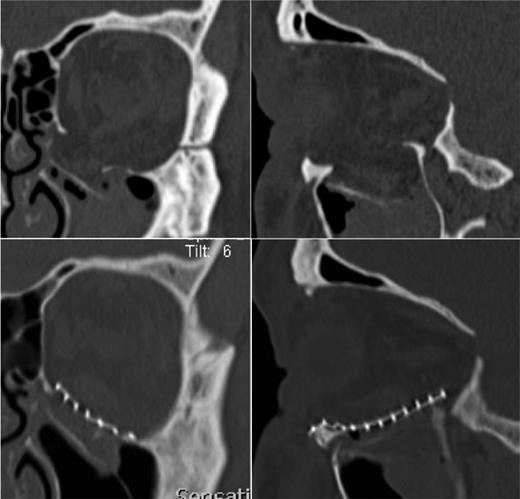
The preoperative (a) and postoperative (b) CT of the left orbital floor fracture showing a satisfactory reposition of periorbital tissue and reconstruction of the orbital floor with a titanium-mesh.
Preoperative forced-duction testing indicated mild restriction in the vertical upward direction, suggesting an entrapment of the IR muscle. Uneventful surgery via a transconjunctival incision was performed under general anaesthesia. The intraoperative finding showed a huge defect of the bone. Therefore, the entrapped orbital tissues were lifted out of the fracture, repositioned and a titanium mesh was inserted for repair of the orbital floor (Fig. 2b).
Four days after surgery, despite good resolution of swelling, there had been essentially no change in the clinical–functional deficit and vertical diplopia persisted due to restriction of infraduction.
A postoperative CT scan showed a good position of the titanium mesh, as well as repositioning of herniated tissues, but highlighted a tear of the IR muscle in its middle part.
Accordingly, the preoperative CT scan was re-evaluated in 0.5 mm slices and the pre-existence of the ruptured IR was shown (Fig. 3). After ophthalmological consultation and treatment of the patient with a combination of orthoptics and prismatic glasses, satisfactory functional recovery was achieved after 6 months without need of surgical repair of the ruptured muscle.
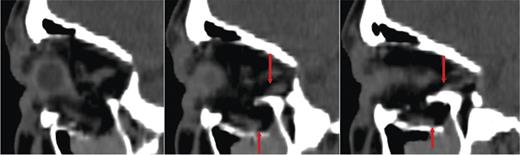
The preoperative 0.5 mm sliced CT of the orbit presents the tear of the IR muscle in his middle part.
DISCUSSION
Orbital fractures are common sequelae of blunt trauma to the periorbital region and can be associated with various ocular and extraocular injuries [3].
Diplopia is not a rare complication and is usually attributed to an incarceration of an extraocular muscle in the orbital fracture site, or a palsy of a cranial nerve or its branch [4].
Inferior and medial rectus muscles are the most commonly involved muscles, an absence of duction and a large deviation with diplopia being the major signs.
Rupture of the IR muscle is also a possible cause of persistent infraduction deficit after blow out fracture. Usually it occurs after penetrating trauma, or secondarily to strabismus or retinal reattachement surgery. It is very rare following blunt orbital trauma [2, 5, 6].
The rectus muscles are more exposed to trauma than oblique muscles, because there is less protective anatomy separating the rectus muscles from the environment [6]. Furthermore, Bell's phenomenon, a protection blink mechanism with an associated upward and most frequently outward movement of the eye, causes these muscles to become more exposed [7, 8].
Ludwig and Brown [1] and Awadein [9] suggested that a possible cause for underaction of IR function is a longitudinal splitting or a flap tear of the muscle. To our knowledge, only two cases of rupture of the IR muscle across its width after blow out fracture were published, in contrast with cases of longitudinal flap tear [1, 2, 5].
In this case, the muscle could have been pressed over the sharp anterior edge of the floor fracture to cause a laceration in its middle part.
Preoperative orbital imaging by a 1 mm-sliced CT scan did not show the tear of the muscle. With the suspicion of muscle incarceration and large fracture of the orbital floor, the indication for surgical reconstruction was given and repair was performed. In the absence of any functional improvement despite a correct surgical repair, a postoperative 0.5 mm-slide CT scan was carried out, which could highlight a tear in the middle part of the rectus inferior belly as the cause of the functional deficit. This fact emphasizes the need for thorough review of the preoperative imaging studies for possible muscle injury in case of orbital fracture.
An isolated traumatic muscle loss is a distressing situation for the patient for both cosmetic and functional results due to diplopia and a compensatory head posture [10].
Reattachment of a ‘snapped’ or torn muscle is the most indicated repair technique for an early diagnosed defect. Ocular realignment can also be achieved with partial or total transposition procedures of the orthogonal rectus muscle with or without recession of the ipsilateral antagonist muscle, or with anterior transposition of the inferior oblique muscle. However, these procedures carry an increased risk of anterior segment ischemia [6, 8]. Prognosis is usually better in patients having partial damage, and treatment options should be evaluated on an individual patient basis [10].
An interdisciplinary team that included the ophthalmologists decided to avoid a second operation and the patient followed an orthoptic treatment with good improvement.
In conclusion, we have described an unusual and rare case of rupture of the IR muscle after blunt orbital trauma. The importance of obtaining a 0.5 mm reconstruction CT scan in blow out fractures with consequent diplopia, to highlight a possible tear of extraocular muscle as the cause, as well as the importance of performing a preoperative forced-duction test, was emphasized. In case of an isolated infraduction deficit after blow out fracture and absence of eye-movement restriction during forced-duction testing, a tear of the rectus inferior muscle has to be suspected. If the CT is normal in spite of persisting diplopia, an MRI may be mandatory for demonstrating the injured muscles [10].



