-
PDF
- Split View
-
Views
-
Cite
Cite
Yazan N. AlJamal, Alan E. Siroy, David R. Farley, A novel approach: chest wall cyst excised by MIS, Journal of Surgical Case Reports, Volume 2013, Issue 9, September 2013, rjt085, https://doi.org/10.1093/jscr/rjt085
Close - Share Icon Share
Abstract
We present a 62-year-old male with a recurrent cyst in the left posterior chest. MRI demonstrated a fluid-filled cavity measuring 23 cm in length and 11 cm in width. The cyst was aspirated demonstrating clear serous fluid. However, the cyst returned and he was referred to us for further treatment. The cyst was excised through a minimally invasive approach using a combination of blunt and electrocautery dissection. The cystic lesion was circumferentially freed from the trapezius muscle and cervical structures. Pathologic examination revealed a benign, fibrous-walled cyst without a true epithelial lining. There are no published reports of a deep thoracic wall cyst resembling this case in terms of histology or location. This patient is free of recurrence 1 year later.
INTRODUCTION
Benign deep thoracic wall cyst is uncommon; however, operative management using an endoscopic approach should be reserved primarily for symptomatic cases with multiple comorbidities, where multiple attempts at aspiration have failed because it is associated with less postoperative pain, lower morbidity and faster recovery [1–4].
CASE REPORT
A 62-year-old Caucasian male presented with swelling and fullness in the left posterior chest. Mild discomfort of the chest wall had worsened over the preceding 6 months. Pain was associated with sitting or leaning against a wall. His range of motion was normal, and he performed daily activities well. Physical examination revealed a morbidly obese white male with a non-tender fluctuant mass on the left side of the upper back. It extended above and below the left scapula. The right side was without abnormality. There were no surgical scars in the thoracic region. The fluctuant mass was the size of a deflated football. An upper midline scar of the neck was noted. The past surgical history included previous cervical spine surgery. The patient had two motor vehicle accidents that caused a lower right-sided lumbar injury. His past medical history was significant for hypertension, hyperlipidemia, sleep apnea, osteoarthritis, gastroesophageal reflux disease and chronic mild asthma.
Computed tomography (CT) scan of the chest demonstrated a large cystic mass between the posterior aspect of the thoracic ribs and deep to the muscles of the left back and scapula. There was no obvious connection with the spinal cord or pleural space. No solid or enhancing component was identified.
Chest magnetic resonance imaging delineated a large cystic mass extending from the level of the lower neck to just above the level of the diaphragm measuring 11 cm transversely, 4.5 cm anteroposteriorly and 23 cm craniocaudally (Fig. 1).
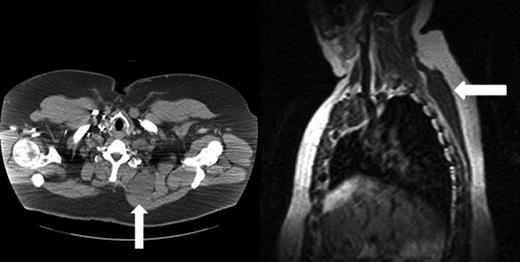
(Left) Chest CT scan shows the large cystic mass (arrow) between the left posterior ribs and muscles of the left back and scapula. No solid or enhancing components are identified. (Right) Chest MRI shows the large cystic mass extending from the level of the lower neck to just above the level of the diaphragm.
The primary care physician aspirated clear fluid under sterile conditions providing symptomatic relief. Cytologic studies were unremarkable. When the mass returned 2 weeks later, he was referred to our institution for further treatment. Due to symptoms referred to the cyst and the lack of response to aspiration, the decision was made to excise the lesion.
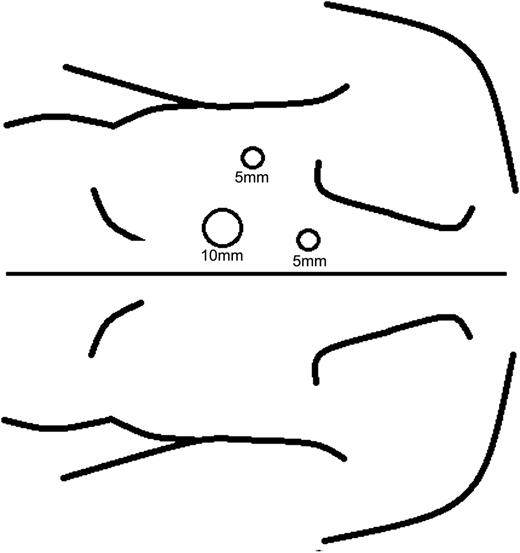
The patient underwent general endotracheal anesthesia and was placed in the right lateral decubitus position. A 2.5-cm longitudinal incision was made at a paramedian position on the left mid-back and it was carried through the level of the fascia by cautery. The paraspinous muscle fibers were separated and the bottom of the cyst was bluntly dissected free and the cyst was aspirated of its serous contents. A balloon dissector was inserted ventral to the cyst for additional blunt dissection. The balloon was inflated to grapefruit size and left inflated for 2 min for hemostasis. The balloon dissector created a larger space beneath the cyst and along its lateral margins. The balloon was then replaced with a Hasson trocar, and two additional 5-mm trocars were placed under direct vision to allow access to the CO2-filled cavity (Fig. 2). Using a combination of blunt and electrocautery dissection, the cystic lesion was circumferentially freed from the trapezius muscle and cervical structures. Several feeding vessels were clipped and divided. Once freed, the cystic mass was removed in its entirety through the Hasson trocar site. Two 15-French round JP drains were inserted through the 5-mm trocar sites and placed to grenade suction.
Intraoperatively, the aspirated cystic fluid was clear and devoid of malignant cells. Histologic analysis of the unilocular cyst revealed a primarily fibrous wall with some adipose tissue and associated vasculature. The cyst lacked a true epithelial lining and any malignant features such as hypercellularity, hyperchromasia, cellular pleomorphism or increased mitoses (Fig. 3). The final pathologic diagnosis was that of a benign, fibrous-walled cyst.
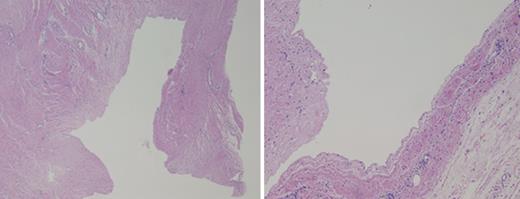
Histology of the cyst shows the lack of a true epithelial lining. No malignant features are visualized.
DISCUSSION
While benign cysts are common within the skin and subcutaneous tissues of the posterior thorax, lesions deep to the muscles are rare. With aspiration of clear fluid devoid of malignant features, the differential diagnosis includes seroma or synovial or ganglion cysts.
Surgical management should be considered for symptomatic patients with unsuccessful multiple times of aspiration. Cysts such as these should undergo aspiration and, if reaccumulation occurs, repeat aspirations with injection of a sclerosing agent or surgical management are reasonable. With the potential need for repeated aspirations and sclerotherapy, our patient opted for cyst removal. Open versus endoscopic surgery was offered. The endoscopic approach was favored in this patient with multiple comorbidities [1–4]. While novel approaches are reported in abdominal wall surgery [1, 3], no reports document this technique for deep chest wall surgery. The balloon dissector and endoscopic resection facilitated free dissection of this large chest wall cyst.
We have found no published reports of a deep thoracic cyst resembling our patient's cyst in terms of histology or location. Such a cyst is obviously rare. The differential diagnosis is not long, consisting primarily of seroma and secondarily of a synovial or ganglion cyst. These entities do not usually have a true epithelial lining, and they tend to occur in areas of previous trauma or surgery. Our patient had undergone previous cervical spine surgery, which conceivably could be the cause of this cystic lesion. However, given its location off the midline, deep-seated nature against the rib cage, and virtually no scarring of the neck near the cyst, we believe that this cyst was unlikely related to the previous operation.
Other diagnoses to consider include sarcoma (which can be ruled out by absence of malignant features on pathology), epidermal inclusion cyst (unlikely given the large size, location deep to the dermal and subcutaneous region, and lack of squamous epithelial lining with keratinization) and abscess (unlikely given absence of inflammatory cells). Given this patient's cyst, it did not fit well into any of the above categories, our pathologists suggest that it is a benign and fibrous-walled cyst. The patient remains asymptomatic and free of recurrence 12 months later.



