-
PDF
- Split View
-
Views
-
Cite
Cite
Hasib Ahmadzai, Darryl Alan Raley, Lynette Masters, Mark Davies, An unusual case of a pituitary fossa aspergilloma in an immunocompetent patient mimicking infiltrative tumour, Journal of Surgical Case Reports, Volume 2013, Issue 4, April 2013, rjt018, https://doi.org/10.1093/jscr/rjt018
Close - Share Icon Share
Abstract
Sellar aspergillosis is a rare infection commonly mistaken for a pituitary tumour. We present a rare case of pituitary fossa Aspergillus fumigatus mycetoma in an immunocompetent 90-year-old female, who presented with headaches. Magnetic resonance imaging scans demonstrated an enhancing pituitary fossa mass that appeared to infiltrate the sphenoid sinus, suggestive of an invasive tumour. Stereotactic trans-sphenoidal resection confirmed localized A. fumigatus infection. The abscess was debrided and the dura was left intact. Her headaches resolved post-operatively and she was treated with voriconazole. This indicates that aspergilloma should be considered as a differential for an unexplained pituitary lesion even in elderly immunocompetent patients.
INTRODUCTION
A pituitary fossa aspergilloma is a potentially life-threatening infection that is often misdiagnosed as it presents with clinical and radiological features similar to pituitary neoplasms. Recognition of the radiological features of these lesions allows early detection, even in rare cases in immunocompetent patients, allowing for appropriate neurosurgical and antifungal therapy.
CASE REPORT
A 90-year-old female presented with 3 months of generalized headaches, anorexia and nausea. She was alert, afebrile, and haemodynamically stable, and neurological examination was unremarkable. Her past medical history included a localized bowel cancer resection and skin melanoma excision several years prior, as well as hypertension. She did not have diabetes mellitus, HIV infection or any previous chemotherapy or immunomodulatory therapies for melanoma. There was no history of craniofacial trauma. Her regular medications included ramipril. Routine investigations including full blood count, serum electrolytes and C-reactive protein were normal. A pituitary hormone screen was normal apart from mildly elevated serum prolactin at 714 mU/ml (normal <536 mU/ml). Routine chest X-ray was also unremarkable.
A computed tomography (CT) brain demonstrated dehiscence of the floor of the sella and mucoperiosteal thickening in the sphenoid sinus with some curvilinear calcification (Fig. 1A). Magnetic resonance imaging (MRI) brain revealed a contrast-enhancing mass within the superior aspect of the sphenoid sinus communicating with the pituitary fossa through the defect of the floor of the sella, measuring 12 mm in maximal craniocaudal dimension. The pituitary gland appeared to be heterogeneous in signal intensity on both pre-contrast T1- and T2-weighted sequences and demonstrated heterogeneous enhancement post-Gadolinium contrast administration (Figs 1 and 2). The imaging findings suggested a pituitary neoplasm with a downward growth pattern. However, the mucoperiosteal thickening in the sphenoid sinuses and the presence of calcification on CT raised the possibility of a mycetoma.
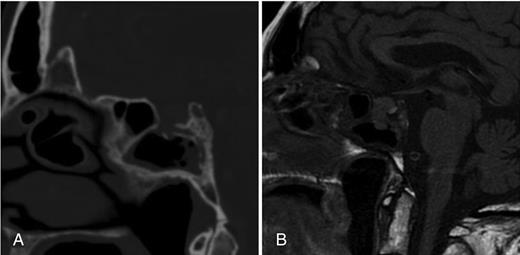
(A) Initial CT scan indicating dehiscence of the floor of the sella and mucoperiosteal thickening in the sphenoid sinus with curvilinear calcification. (B) Initial T1-weighted MRI, indicating a pituitary fossa mass communicating with the superior aspect of the sphenoid sinus.
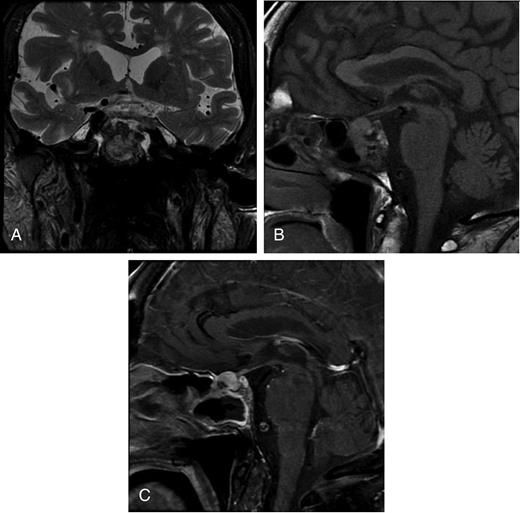
MRI performed 3 weeks after initial presentation. (A) T2-weighted MRI coronal section displaying an expanding, infiltrative pituitary fossa mass. (B) T1-weighted MRI sagittal view, indicating that the lesion is locally infiltrating the sphenoidal sinus. (C) Post-gadolinium sagittal T1-weighted MRI indicating a heterogeneously enhancing mass.
The patient's headache worsened despite management with simple analgesia. A repeat MRI performed 3 weeks after presentation demonstrated that the lesion had expanded in size and appeared to be breaching the diaphragma sella, with extension to the inferior surface of the optic chiasm (Fig. 2).
The patient underwent stereotactic-guided endoscopic transnasal transsphenoidal surgery. The sphenoidal sinus mucosa was exenterated via an endoscopic endonasal incision, and abnormal irregular friable yellow tissue was removed from clival and sella portions of the posterior wall of the sphenoidal sinus. Invasive fungal hyphae were demonstrated on histopathological frozen section. There was no evidence of dural extension and the remaining abscess material was removed without breaching dura. Post-operatively, amphotericin-B was initiated. Fungal cultures of the biopsy specimens later identified the growth of Aspergillus fumigatus, and she was initiated on 400 mg/day oral voriconazole. The patient's headaches resolved almost completely after the operation. Her post-operative course was complicated by visual and tactile hallucinations and hyponatremia (Na+ 123 mmol/l). Serum and urine osmolalities were 261 mmol/kg (normal 280–303 mmol/kg) and 439 mmol/kg, respectively, and the urinary sodium was 41 mmol/l. The patient remained euvolaemic and there was no post-operative polyuria. The patient's cortisol level was 665 nmol/l (normal 155–600 nmol/l) and thyroid-stimulating hormone level was 1.1 mU/l (normal 0.1–3.8 mU/l). The hyponatraemia and hallucinations were believed to be the result of a syndrome of inappropriate anti-diuretic hormone syndrome (SIADH), a complication of surgery of the sellar region and possibly also a side-effect of the voriconazole, which was temporarily withheld. She was given risperidone, which resolved her hallucinations. Three months after surgery, the patient had no neurological complaints. Repeat MRI at this stage showed persisting mucoperiosteal thickening with post-surgical changes in the sphenoid sinus, but no evidence of a mycetoma.
DISCUSSION
Aspergillus fumigatus commonly causes infection in immunocompromised patients, with central nervous system (CNS) aspergillosis having a mortality as high as 90% if untreated [1, 2]. It may present as meningitis, encephalitis, cerebral or subdural mycetoma, mycotic arteritis or pituitary mycetoma [1, 3]. Although Aspergillus infection of the paranasal sinuses is well recognized, aspergilloma involving the pituitary gland and sella are exceedingly rare in immunocompetent individuals. Patients with aspergillosis typically have underlying immunosuppression, including diabetes mellitus, granulocytopenia or prolonged hospitalization [1]. Although our patient was not immediately immunocompromised, advanced age is, however, an immuno-compromising factor.
Aspergillus can reach the CNS by either direct haematogenous spread; local invasion from extracranial locations; or iatrogenic neurosurgical introduction [1, 2]. Of note, the patient in this case had radiological evidence of sphenoidal sinusitis, which predisposed to mycetoma formation. The communication from the sphenoidal sinus to the sella turcica through vascular channels may be the possible route of spread [1, 3].
In the first reported case of pituitary aspergillosis, the patient died from diffuse Aspergillus meningo-encephalitis following treatment with transfrontal craniotomy [1]. Owing to the high mortality associated with CNS aspergillosis, early diagnosis and management is critical. Pre-operative clinical presentations with headaches, pituitary dysfunction and ophthalmological signs are similar to those in neoplasms, making diagnosis problematic. CT and MRI remain the best techniques for pre-operative diagnosis.
This case highlights key neuroradiological diagnostic pearls for pituitary aspergillomas. Specific radiological features evident in this case include iso-to-hypointense signals on T1-weighted sequences, heterogeneous enhancement on post-gadolinium T1-weighted sequences and hypointensity on T2-weighted images [3, 4]. Hypointensity on T2-weighted images is a key feature of an aspergilloma, indicating high concentrations of ferromagnetic elements including iron, zinc, magnesium and manganese, critical for fungal amino-acid metabolism [2]. However, unlike previous cases, the mycetoma in this patient did not demonstrate a rim of peripheral ring enhancement [1–3]. Other important features of pituitary mycetomas on CT scans include mucoperiosteal thickening, bony erosion and calcification within the lesion [4]. These imaging features help in distinguishing these lesions from pituitary neoplasms. Pituitary adenomas are classically isointense on T1-weighted images and enhance homogenously post-contrast. If one is faced with an unusual pituitary lesion, including hypointensity on T2-weighted images, contiguous osteomyelitis or sinusitis, then an infectious process should be considered.
Despite the patient's advanced age, she tolerated the operation well with a favourable outcome. It would have been unconscionable given her age to dismiss the pituitary lesion as a neoplastic process, missing the diagnosis and failing to cure the patient. In this case, extradural resection of the mycotic mass ensured histopathological diagnosis and prevented fatal outcomes including dural extension and cerebrospinal fluid contamination [5]. Post-operative systemic antifungal therapy is important in preventing subsequent meningoencephalitis or vasculitis. Large-scale clinical trials have indicated superiority of voriconazole over amphotericin-B for first-line therapy in patients with aspergillosis in terms of survival, response rates and safety [2]. However, this case also highlighted rare adverse-effects of voriconazole-associated hallucinations and hyponatremia, indicating the need for therapeutic voriconazole concentration monitoring. The patient's hyponatraemia was believed to be the result of SIADH resulting from manipulations of the pituitary stalk from operating on the sellar region, although voriconazole has been observed to be a contributing factor [6].
This case highlights a rare presentation of pituitary aspergilloma in an elderly, otherwise immunocompetent woman, illustrating the importance of considering aspergilloma in the differential diagnosis of a sellar mass. Transsphenoidal surgical debridement along with antifungal therapy is critical in ensuring patient survival and optimal outcome.



