-
PDF
- Split View
-
Views
-
Cite
Cite
Rohit Singh, Thomas Moores, Mark Maddox, Andrew Horton, Internal iliac aneurysm presenting with lower back pain, sciatica and foot drop, Journal of Surgical Case Reports, Volume 2013, Issue 2, February 2013, rjs032, https://doi.org/10.1093/jscr/rjs032
Close - Share Icon Share
Abstract
Internal iliac aneurysms are usually silent and are identified as an incidental finding on a radiological investigation for an unrelated condition, unless catastrophic bleeding occurs. We present the first case of a middle-aged man with a large internal iliac aneurysm presenting with a foot drop and sciatic nerve pain. The endovascular management is discussed.
INTRODUCTION
Isolated aneurysms of the internal iliac are extremely rare and are seen as a variant of aorto-iliac aneurysm disease. The incidence of isolated internal iliac aneurysms is around 0.04% of all aorto-iliac aneurysms [1]. The detection of internal iliac aneurysms is usually coincidental, but it has been reported that up to 40% present acutely with rupture [2]. Symptoms presenting with internal iliac aneurysms included abdominal pain (31.7%), urological symptoms (28.3%), neurological symptoms (18.3%), groin pain (11.7%), hip or buttock pain (8.3%) and Gastrointestinal symptoms (8.3%) [1, 2]. The gold standard for surgical repair is open interstitial graft repair, which carries a mortality of up to 10% [3]. Minimally invasive endovascular repair is being increasingly performed in appropriately selected patients [3–5]. We present the first case of a gentleman presenting with foot drop and sciatica caused by an aorto-iliac aneurysm, which was successfully treated with endovascular repair.
CASE REPORT
A 64-year-old lorry driver, with a past medical history of hypertension controlled with valsartan, was referred by his General Practitioner (GP) to fracture clinic with lower left-sided back and sciatic nerve pain with numbness to the outer aspect of the foot.
He had initially been seen by his GP 3 weeks earlier complaining of lower back pain, dysuria and urinary frequency. Urine dipstick showed blood and protein and his urinary symptoms had settled with a 7-day course of trimethoprim. He had continued worsening lower back pain, so a full myeloma screen was organized including lumbar spine radiographs. Follow-up urinalysis was unremarkable, calcium was 2.62 (range 2.1–2.6), alkaline phosphatase was 134 (range 43–114) and ESR was 100, lumbar radiographs and PSA were normal, and Bence Jones Electrophoresis was awaited.
Following a further review by the GP, he was now complaining of increasing lumbar back pain with associated limp but no neurological deficit, and feeling systemically unwell, so he was referred to the orthopaedic team for an urgent review for suspected myeloma or bony metastasis.
Orthopaedic review detected sensory loss in the S1 dermatome and foot drop on the left side. He was clinically well. Urgent magnetic resonance imaging (MRI) demonstrated a 9 cm left iliac aneurysm in contact with the left L5 nerve root and in close proximity to the S1 nerve root (Figure 1a and b). There was also left ureteric dilatation with hydronephrosis. The spinal cord was normal.
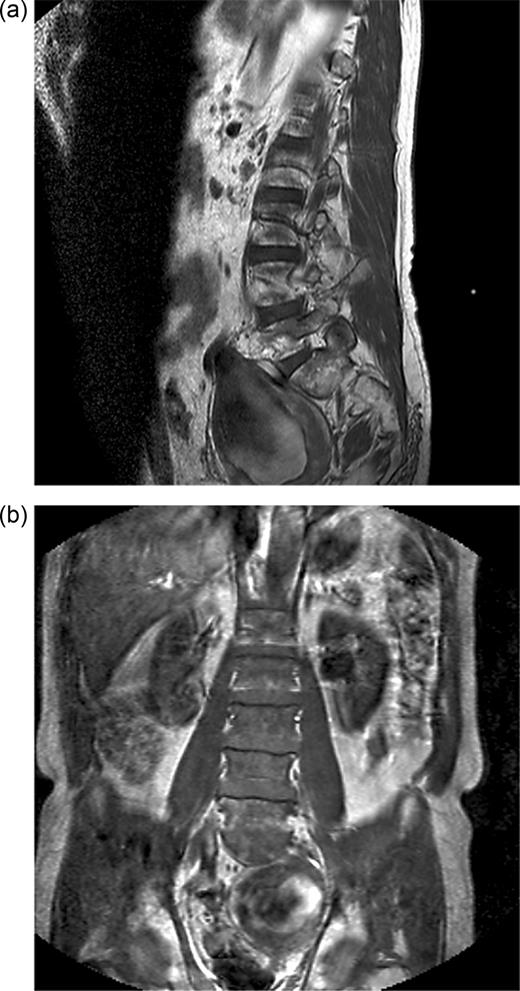
(a) T1-weighted sagittal MRI showing internal iliac aneurysm. (b) T1-weighted coronal MRI showing internal iliac aneurysm.
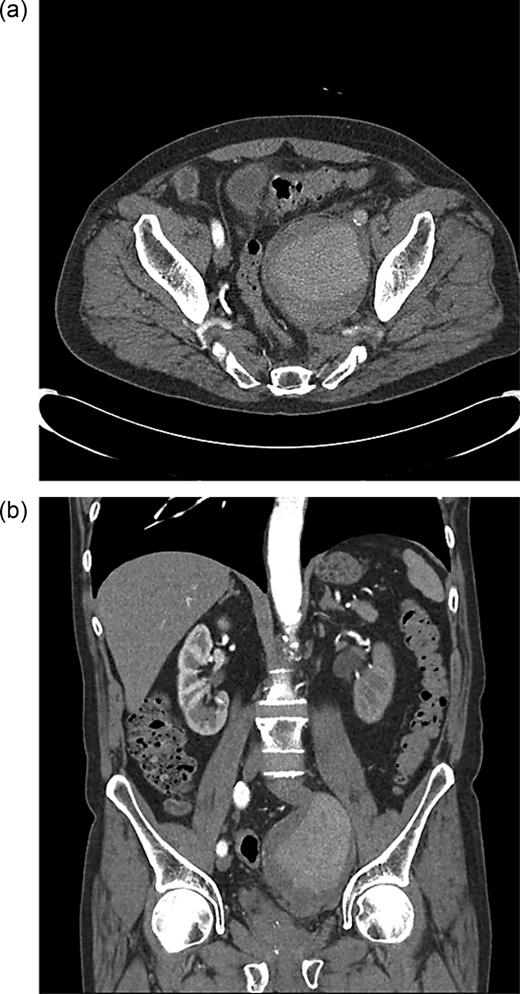
Computed tomography (CT) angiography was requested, and the patient was started on antibiotics because of the concerns over a mycotic aneurysm after discussion with the vascular team. CT angiography showed the internal iliac aneurysm obstructing the left ureter and abutting local nerve roots, with atheromatous disease within the common femoral arteries with an ectatic aorta (Figure 2a and b).
The radiologists proceeded to perform endovascular embolization of the left internal iliac to aid any further procedures. It was during direct catheterization of this aneurysm that it was noted to be blind ending with cross filling of the posterior division of the left internal iliac artery via collaterals from the right internal iliac artery (Figure 3a and b).
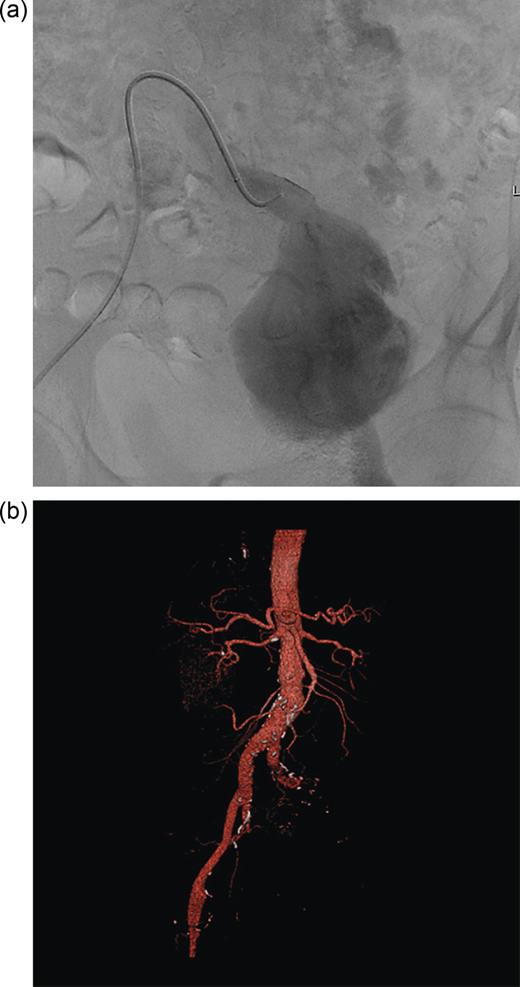
(a) Endovascular catheterization showing aneurysm to be blind ending. (b) 3D CT reconstruction showing blind ending aneurysm.
As a result, the aneurysm was managed by passing a stent graft from the left common iliac artery; this was extended with a second graft down into the distal external iliac artery.
The patient was discharged 2 days later with a foot-drop splint and outpatient physiotherapy to manage his peroneal nerve injury causing foot drop.
Six weeks later, CT imaging showed a reduction in sac size although the patient was still having intermittent nerve root pain and the foot drop was still present.
DISCUSSION
We present an unusual case of aorto-illiac aneurysm presenting with a back pain, sciatica and foot drop. The concern in this case was that of a musculoskeletal malignancy, with unstable progressive neurology. This highlights the importance of appropriate investigations, in the form of an urgent MRI to investigate a cause for progressive neurology, which incidentally determined the underlying diagnosis.
Furthermore, traditional management for internal iliac aneurysms is by open interposition graft surgical repair, which remains the gold standard [2], with the primary indication for repair being to prevent rupture in an aneurysm >4 cm in diameter [2–3, 6]. This is a major operative procedure, usually performed in a semi-elective setting unless acutely presenting with rupture. It carries significant morbidity and mortality of up to 10% [3], owing to the difficult dissection and surgical approach into the pelvis with high risk of visceral, genitourinary and pelvic venous injury. With the advancement of endovascular techniques, over the last 10–15 years has been shown to be safe and effective in many retrospective case series [3–5] and is especially useful in those with challenging anatomy. In our case, the aneurysm involved the left lumbosacral plexus, which could have made open repair challenging with a high risk of further neurological damage. We have shown that minimally invasive repair has an important role in managing isolated aneurysms of this type for patients with an appropriate anatomy. Furthermore, this technique has minimized the hospital stay, which is evident by our patients' 2-day hospital admission, which is significantly less than with an open repair, with reported the length of stay being between 7 and 14 days [1, 3–7].
The patient is still symptomatic with a foot drop; we can attribute the neurological symptoms to the aneurysms anatomy at presentation, which may also have remained or deteriorated after open repair, but endovascular repair avoided the increased associated morbidity with an open approach [7]. He remains under follow-up for the foot drop and sciatica; the sciatica symptoms are improving, and the foot drop may recover now the aneurysm has started to reduce in size, or he may require long-term orthotic treatment.
Conflict of interest: None declared.



