-
PDF
- Split View
-
Views
-
Cite
Cite
Svetlana Kleyman, Shafia Ashraf, Sherin Daniel, Dinesh Ananthan, Aliu Sanni, Feroze Khan, Pericecal hernia: a rare form of internal hernias, Journal of Surgical Case Reports, Volume 2013, Issue 2, February 2013, rjs021, https://doi.org/10.1093/jscr/rjs021
Close - Share Icon Share
Abstract
We report a rare and interesting case of a pericecal hernia. A 34-year-old male presented to the emergency department with severe periumbilical pain, emesis and a prior syncopal episode. He noted a 3-month history of intermittent, colicky periumbilical pain. His abdominal examination demonstrated a palpable mass in the right lower quadrant, involuntary guarding and rebound tenderness. CT demonstrated dilated small-bowel loops and findings suggestive of ischemia. The patient was immediately taken to the operating room where a diagnosis of pericecal hernia was made. The patient underwent a reduction of the hernia and a repair of the mesenteric defect.
INTRODUCTION
Internal hernias are protrusions of a viscus through a peritoneal or mesenteric aperture. The overall incidence is less than 1%; however, they can contribute to 5.8% of small-bowel obstructions. One rare type of internal hernia is a pericecal hernia. Pericecal hernias present as colicky right lower quadrant pain and symptoms of small-bowel obstruction. Once the diagnosis is made, the treatment is immediate operative intervention to prevent severe complications such as bowel strangulation and necrosis.
CASE REPORT
A 34-year-old man presented to the emergency department after a low velocity motor vehicle accident. He complained of severe periumbilical pain, emesis and an episode of syncope 7 hours prior at arriving to the hospital. He described his abdominal pain as constant, radiating to the right lower quadrant and associated with nausea and vomiting. His last bowel movement was prior to his presentation to the hospital. The patient described a history of intermittent, colicky periumbilical pain for the past three months. He denied any previous surgical history. He had no history of any tobacco, alcohol or recreational drug use. On physical examination, the patient was afebrile with a blood pressure of 132/76 and pulse rate of 68. Abdominal examination revealed no signs of abdominal trauma or previous surgical scars. He had a tender palpable mass in the right lower quadrant with involuntary guarding and rebound tenderness. His white blood cell count was 9 × 103/µl, and his venous lactate level was 2 mmol/l. Computed tomography of his abdomen and pelvis was done (Fig. 1). A provisional diagnosis of acute abdomen with small-bowel obstruction was made. In view of his abdominal examination and findings on the CT scan, he was taken to the operating room for an exploratory laparotomy. An encased mass of small bowel was found twisted on itself through a vent in the mesentery (Fig. 2). It initially appeared dusky but became viable after reduction and repair of the mesenteric defect. This was consistent with an internal hernia of the pericecal type.
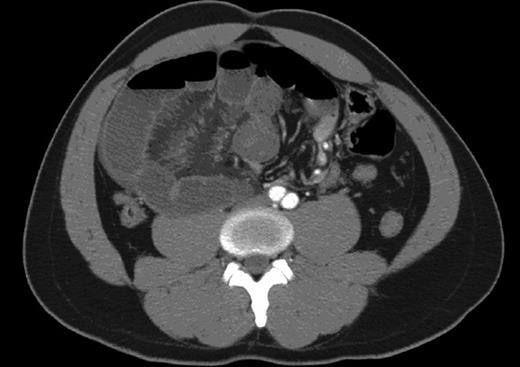
This CT demonstrates dilated small-bowel loops and a whirling sign suggestive of mesenteric and bowel congestion with bowel thickening consistent with ischemia.
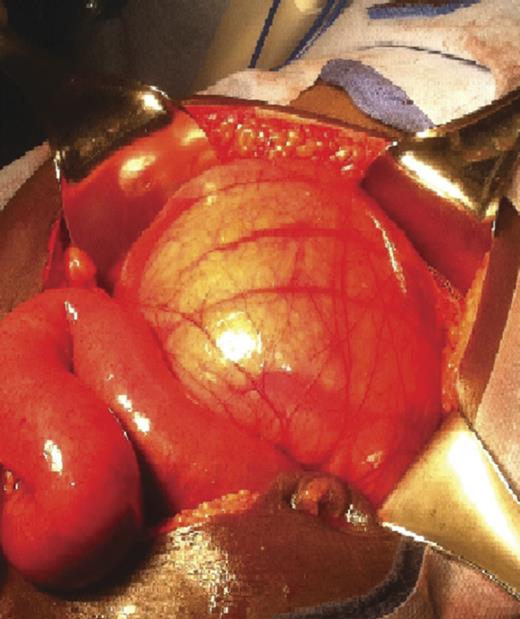
Intra-operative findings demonstrating a distended small bowel mass, enclosed in a membrane, which was encountered on entering the peritoneum.
DISCUSSION
Internal hernias are defined as the protrusion of a viscus through a peritoneal or mesenteric aperture. The overall incidence is <1%; however, they constitute 5.8% of all small-bowel obstructions [1]. Defects in the visceral peritoneum and mesentery occur due to congenital, surgical, traumatic, inflammatory or circulatory pathology. If left untreated, the overall mortality rate exceeds 50% [2]. There are some small and easily reducible hernias that can remain relatively asymptomatic during life. Clinical manifestations include a history of intermittent attacks of vague epigastric discomfort associated with feelings of distention, colicky periumbilical pain, nausea and vomiting after large meals. Internal hernias should be suspected in patients with signs and symptoms of intestinal obstruction in the absence of inflammatory intestinal diseases, external hernias or previous laparotomy. Pericecal hernias account for 13% of all internal hernias. These hernias develop in one of the four peritoneal fossae (superior ileo-cecal, inferior ileo-cecal, retro-cecal and paracolic sulci) [2]. They occur when the herniated loop consists of an ileal segment that protrudes through a defect in the cecal mesentery and extends into the right paracolic gutter. These hernias can be diagnosed on plain radiographs due to the abnormal relationship of the ileum to the cecum in association with signs of small-bowel obstruction. CT findings demonstrate dilatation of small intestine loops with a transitional zone adjacent to the cecum or thickened small intestine lateral to the cecum. This type of hernia is commonly associated with a rapid progression to strangulation and the mortality rate can be as high as 75% [1]. Making a prompt diagnosis and initiating definitive surgical management is mandatory in these cases to avoid complications [3]. The surgical approach for internal hernias includes reduction of the herniated intestinal contents, resection of any necrotic bowel and closure of the hernia defect.



