-
PDF
- Split View
-
Views
-
Cite
Cite
James Paget, Neil Patel, Jacob Manushakian, Ulnar nerve compression in Guyon's canal: MRI does not always have the answer, Journal of Surgical Case Reports, Volume 2013, Issue 1, January 2013, rjs043, https://doi.org/10.1093/jscr/rjs043
Close - Share Icon Share
Abstract
Lipoma is a rare cause of ulnar nerve compression in Guyon's canal. All four previously reported cases from 2000 to 2009 have been accurately diagnosed on MRI. We present a case report where the MRI and surgical findings differed and a summary of the previous cases in the literature. We conclude that although MRI remains the best investigation for this condition, it is not always accurate and clinical findings still provide the best basis for surgical treatment.
INTRODUCTION
Aetiologies of ulnar nerve compression at the wrist include ganglia, fractures, anomalous muscles, thrombosis, bursitis, a thick pisohamate ligament and lipomas. To date there have been six case studies reporting compression in Guyon's canal secondary to lipoma [1–6].
CASE REPORT
A right-handed 37-year-old man presented with paraesthesia and altered sensation on the volar aspect of his left ring and little fingers. Although Froment's sign was negative, he had generalized weakness affecting the middle finger and thumb compared with the right hand. This had been present for 2 years. He had had previous surgery for a ganglion on the radial aspect of his left wrist. Clinical examination was otherwise normal.
Nerve conduction studies demonstrated no definite peripheral ulnar nerve lesion at the wrist or elbow. However, ulnar mixed nerve responses were slightly reduced in amplitude.
A T1-weighted and STIR (short T1 inversion recovery) MRI scan of the wrist, reconstructed in axial and coronal planes was performed (Fig. 1). This showed no obvious deformity in Guyon's canal and no abnormality along the ulnar nerve. However, it did demonstrate a multi-loculated ganglion along the volar aspect of the distal radius closely abutting the radio-carpal ligament and a fatty mass superficial to the roof of Guyon's canal. As the patient had persistent hand symptoms, we proceeded to surgically explore his wrist.
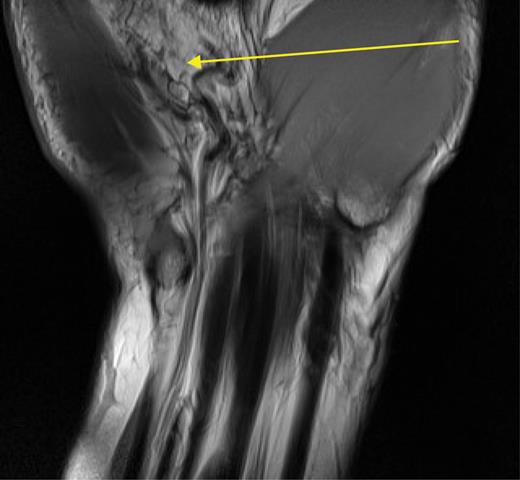
T1-weighted MRI scan of Guyon's canal. The arrow indicates the fatty mass reported as lying atop Guyon's canal.
The ganglion was first excised from the radial aspect of the volar wrist and the median nerve was then released in the carpal tunnel. The incision was extended medially and Guyon's canal was explored. A multi-lobulated piece of fatty tissue was found within the canal measuring 3 cm × 2 cm × 1.5 cm (Fig. 2). This was compressing the ulnar nerve. This was removed and histological analysis showed mature adipose tissue consistent with lipoma.
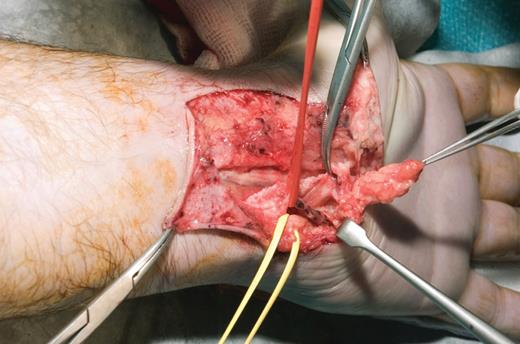
Operative pictures of Guyon's canal: lipoma in forceps, yellow sloop around nerve, red sloop around the ulnar artery.
The ulnar nerve was intact throughout its course in the canal with no macroscopic pathology. The ulnar artery was also intact with no evidence of thrombosis.
The patient made a good postoperative recovery and his symptoms resolved completely over the following 4 months.
DISCUSSION
Ulnar nerve compression from lipoma in Guyon's canal is rare. Our literature search found six cases of this reported previously [1–6]. In all cases, surgical excision of the lipoma led to good relief of ulnar nerve symptoms. Our case is clinically similar with the removal of the lipoma leading to relief of ulnar nerve symptoms.
Sakai et al. [3] were the first to report the use of MRI in their work-up for compressive lipoma in Guyon's canal in 2000. Since then MRI has been the most useful diagnostic investigation, with good correlation between the imaged and surgical findings (Table 1). However, in our case, the MRI scan interpretation was inconclusive and did not correlate accurately with the surgical findings. At surgery, the lipoma was found in Guyon's canal, not superficial to it.
Summary of MRI and surgical findings in case reports of compressive lipoma in Guyon's canal (1971–2009)
| Report . | MRI . | Reported protocol . | MRI correlation with surgery . |
|---|---|---|---|
| McFarland and Hoffer (1971) [1] | No | n/a | n/a |
| Zahrawi (1984) [2] | No | n/a | n/a |
| Sakai et al. (2000) [3] | Yes | T1 and T2-weighted MRI axial reconstruction | Yes |
| Bui-Mansfield et al. (2002) [4] | Yes | T1-weighted MRI axial and coronal reconstructions | Yes |
| Gruber and Towfigh (2002) [5] | Yes | T1-weighted MRI sagittal and coronal reconstructions | Yes |
| Rohila et al. (2009) [6] | Yes | T1- and T2-weighted MRI and SITR (coronal and axial imaging reconstruction) | Yes |
| Report . | MRI . | Reported protocol . | MRI correlation with surgery . |
|---|---|---|---|
| McFarland and Hoffer (1971) [1] | No | n/a | n/a |
| Zahrawi (1984) [2] | No | n/a | n/a |
| Sakai et al. (2000) [3] | Yes | T1 and T2-weighted MRI axial reconstruction | Yes |
| Bui-Mansfield et al. (2002) [4] | Yes | T1-weighted MRI axial and coronal reconstructions | Yes |
| Gruber and Towfigh (2002) [5] | Yes | T1-weighted MRI sagittal and coronal reconstructions | Yes |
| Rohila et al. (2009) [6] | Yes | T1- and T2-weighted MRI and SITR (coronal and axial imaging reconstruction) | Yes |
Summary of MRI and surgical findings in case reports of compressive lipoma in Guyon's canal (1971–2009)
| Report . | MRI . | Reported protocol . | MRI correlation with surgery . |
|---|---|---|---|
| McFarland and Hoffer (1971) [1] | No | n/a | n/a |
| Zahrawi (1984) [2] | No | n/a | n/a |
| Sakai et al. (2000) [3] | Yes | T1 and T2-weighted MRI axial reconstruction | Yes |
| Bui-Mansfield et al. (2002) [4] | Yes | T1-weighted MRI axial and coronal reconstructions | Yes |
| Gruber and Towfigh (2002) [5] | Yes | T1-weighted MRI sagittal and coronal reconstructions | Yes |
| Rohila et al. (2009) [6] | Yes | T1- and T2-weighted MRI and SITR (coronal and axial imaging reconstruction) | Yes |
| Report . | MRI . | Reported protocol . | MRI correlation with surgery . |
|---|---|---|---|
| McFarland and Hoffer (1971) [1] | No | n/a | n/a |
| Zahrawi (1984) [2] | No | n/a | n/a |
| Sakai et al. (2000) [3] | Yes | T1 and T2-weighted MRI axial reconstruction | Yes |
| Bui-Mansfield et al. (2002) [4] | Yes | T1-weighted MRI axial and coronal reconstructions | Yes |
| Gruber and Towfigh (2002) [5] | Yes | T1-weighted MRI sagittal and coronal reconstructions | Yes |
| Rohila et al. (2009) [6] | Yes | T1- and T2-weighted MRI and SITR (coronal and axial imaging reconstruction) | Yes |
MRI scanning is now well established as the most accurate diagnostic method for peripheral nerve lesions and for soft tissue lesions around the wrist using T1 and STIR sequences with two plane reconstructions [7–9]. It is also recognized that higher Tesla MRI machines have greater scanning resolution. However, our unit's 1.5 Tesla MRI may not have been able to distinguish the exact location of the lipoma in this complex anatomical region.
In our opinion, the persistence of ulnar nerve symptoms in the patient necessitated surgical exploration in spite of relatively negative, inconclusive investigations. We believe that the old maxim of ‘treating the patient not the scan’ still holds true, particularly when anatomically small, rare causes can sometimes be overlooked by even the best available tests.
Conflict of interest statement. None declared.



