-
PDF
- Split View
-
Views
-
Cite
Cite
M Alibhai, I Balasundaram, C Bridle, Cutaneous sinuses of dental origin, Journal of Surgical Case Reports, Volume 2012, Issue 8, August 2012, Page 6, https://doi.org/10.1093/jscr/2012.8.6
Close - Share Icon Share
Abstract
We report a case of a cutaneous sinus related to a non-vital lower premolar. The case was misdiagnosed by non-dentally trained medical staff and subsequent treatment proved ineffective. Following referral to an Oral and Maxillofacial clinic the correct cause was established. Correct treatment was followed by rapid resolution of signs and symptoms.
This case highlights the need for healthcare professionals dealing with such patients to be aware of the dentition as a cause for cutaneous sinuses in the head and neck region. Those professionals not dentally qualified should enquire about dental pain and consider referral to the dental practitioner or a specialist department for further evaluation. Even those with a dental background can be fooled and a through history and examination is paramount, supplemented by special investigations were appropriate.
INTRODUCTION
A cutaneous sinus of dental origin is a relatively uncommon occurrence and may be easily misdiagnosed. They do not always arise close to the underlying infection and dental symptoms may be absent (1). Often patients seek care from general physicians and surgeons with other diagnoses being made such as furuncles, basal cell and squamous cell carcinomas. It has been estimated that half of all patients undergo surgical excisions, multiple biopsies, antibiotic courses and even radiotherapy before definitive diagnosis (1,2,3).
Misdiagnosis worsens the chronicity of the lesion and has pronounced effects on facial aesthetics due to unnecessary treatments resulting in further skin scarring. Once the correct diagnosis is made, definitive treatment, through either tooth extraction or root canal therapy to eliminate the source of infection, is simple and effective.
CASE REPORT
A 40-year-old male presented to the Oral and Maxillofacial Surgery department with a 3-year history of a cutaneous sinus affecting the left cheek.
He complained of intermittent swelling affecting the left face with a discharge of pus onto the left cheek. He denied any history of pain. He had suffered an alleged assault 3 years prior and was struck with fists and glass bottles to the left face. He had assumed his symptoms were a result of this attack.
He suffered no other medical conditions, did not take any medications and had no allergies. He smoked 10 cigarettes a day and seldom drank alcohol. He lived with family and worked as a school caretaker. He had only recently registered with a dentist.
In the 12 months prior to his presentation the patient had been referred to a local Plastic Surgery department via his General Medical Practitioner and had received treatment with no resolution of symptoms. The lesion was refractory to oral antibiotics and he had undergone excision biopsy of the cutaneous sinus followed by a Z-plasty scar revision.
On examination there was scarring to the left mental region with evidence of previous revision surgery and a draining cutaneous sinus (Fig. 1 & 2).

showing scarring to the left mental region with evidence of previous revision surgery and a draining cutaneous sinus
Intra-orally there was a crowned lower left first premolar which was not tender to percussion. There were no mucosal lesions or buccal sulcus swelling or tenderness.
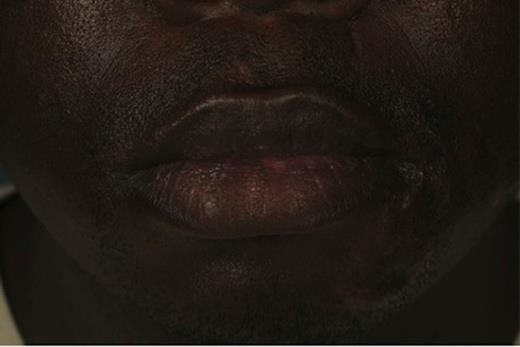
Image showing scarring to the left mental region with evidence of previous revision surgery and a draining cutaneous sinus
Plain radiographs revealed a periapical radiolucency of the lower left first premolar. A gutta percha (GP) point was inserted into the sinus. Cone beam computed tomography (CBCT) showed the GP point to be in communication with the periapical area (Fig. 3 & 4).
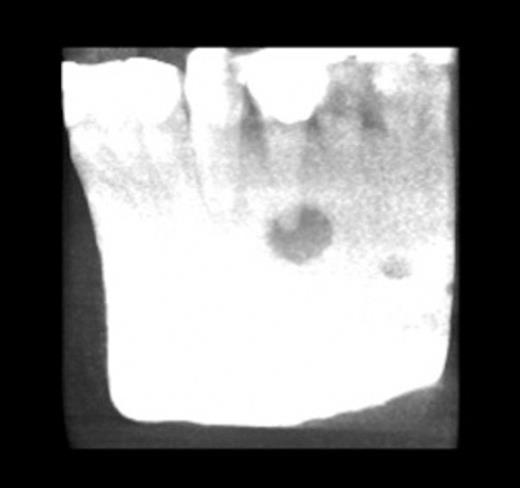
CT showing gutta percha point communicating with the periapical area
He was diagnosed with an oral cutaneous sinus associated with a non-vital lower left first premolar. Pulp extirpation was undertaken and with completion root canal treatment by the dental practitioner.
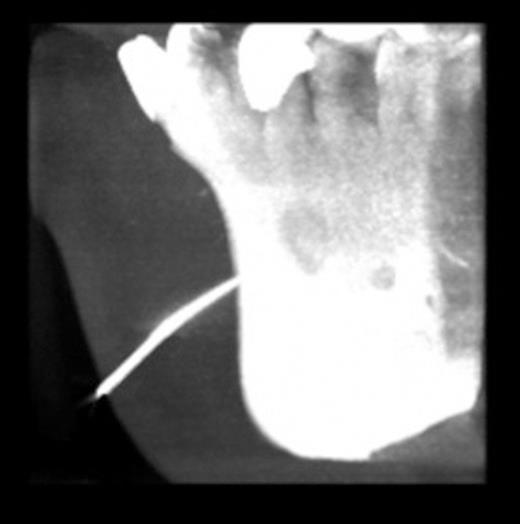
CT showing gutta percha point communicating with the periapical area
DISCUSSION
A cutaneous dental sinus is a channel that leads from a dental focus of infection to drain onto the face or neck (2). They are typically formed by periapical abscesses, which result from inflammatory degeneration of the pulp and periodontal membrane (4). The inflammatory and immunological processes then induce bone resorption, resulting in the formation of an intraoral or cutaneous sinus. The point of drainage usually depends on the location of the apex of the affected tooth in relation to the muscular attachments of the bone and will follow the path of least resistance through the fascial planes of the face (5).
Approximately 80% of cutaneous sinuses that occur arise from mandibular teeth and thus appear on the chin or submental region (6). Rarely, a dental cyst or un-erupted tooth can be the source of the infection. A retained root fragment can be the cause in edentulous patients.
Recognition of a sinus tract can present a diagnostic problem. Lesions may resemble a pyogenic granuloma, actinomycosis, a thyroglossal duct cyst, a branchial cleft cyst, a furuncle, a squamous cell carcinoma and an epidermal cyst (1).
Careful questioning of the patient about past symptoms may help identify a dental cause but symptoms may not be present in all cases. Sinus tracts are most commonly found on the chin, submental region or in the submandibular area (7). The characteristic lesion is an erythematous, soft nodule fixed to underlying structures. There is periodic drainage and crusting in some cases and the lesion is depressed below the normal skin surface. Palpation of the surrounding tissue may produce pus, which supports the diagnosis.
Intraoral examination is critical for making the diagnosis. In particular, the examiner should look for dental caries or restorations and periodontal disease. Vitality testing of potentially causal teeth should be undertaken. Radiographs will show a radiolucency at the apex of the infected tooth. A GP point can be used to trace the sinus tract to its origin, which is usually a nonvital tooth.
Biopsy, if performed, will show nonspecific findings such as hyperplasia and chronic inflammation (8). Once the correct diagnosis is made, root canal therapy or surgical extraction is the treatment of choice and antibiotics may be used as an adjunct to surgical therapy.
The sinus tract usually disappears in 5 to 14 days (9). Dimpling and hyperpigmentation of the area are not uncommon and usually fade with time. Surgical revision of the scar can be undertaken to provide better a cosmetic result. Failure of a cutaneous sinus tract to heal after adequate root canal treatment or extraction requires further evaluation and biopsy.
As in this case, cutaneous sinuses of dental origin are often misdiagnosed and inappropriately treated. Patient dissatisfaction following such diagnostic and therapeutic misadventures is understandably high. Clinicians should be aware of the fact that any cutaneous lesion of the face and neck can be of dental origin and should seek communication and evaluation from appropriate specialists and general dental practitioners.



