-
PDF
- Split View
-
Views
-
Cite
Cite
P Kambakamba, M Lesurtel, S Breitenstein, MY Emmert, MJ Wilhelm, PA Clavien, Giant mesenteric cystic lymphangioma of mesocolic origin in an asymptomatic adult patient, Journal of Surgical Case Reports, Volume 2012, Issue 6, June 2012, Page 4, https://doi.org/10.1093/jscr/2012.6.4
Close - Share Icon Share
Abstract
A 34-year-old patient was scheduled for valve replacement to treat a symptomatic mitral regurgitation. The preoperative work-up incidentally discovered an intra-abdominal cystic tumour extending from the epigastrium to the pelvic region on a computed tomography scan. The patient had no abdominal symptoms by the giant cyst from unkown origin. An open “en bloc” resection disclosed a large cyst in the mesocolon. Pathological examination, including immunohistochemistry, enabled the diagnosis of a mesenteric cystic lymphangioma. Long-term follow-up of 12 months shows no recurrence. Mesenteric cystic lymphangioma, which is extremely rare in adults, is a challenge to diagnose and needs complete resection to ensure dignity and to avoid recurrence.
INTRODUCTION
Lymphangiomas are malformations of the lymphatic drainage system and mostly occur in childhood. The localization of these cystic tumours is mainly the cervical or axillary region; in addition there are rare reports regarding their occurrence in the mediastinum, in the retroperitoneum as well as in the abdominal cavity appearing as mesenteric cysts. With an estimated incidence of 1/1000000 and fewer than 200 cases described in literature the mesenteric form in adults represents a very rare entity. Here, we present one case of a giant mesenteric cystic lymphangioma in an asymptomatic patient
CASE REPORT
A 34-year-old patient was scheduled for minimal invasive mitral valve reconstruction to treat a Barlow syndrome with a prolapse of the posterior mitral leaflet. The patient’s medication consisted of a Proton pump inhibitor due to a chronic gastro-esophagial reflux disease. Otherwise the patient had no other digestive symptoms, in particular there was no history of pancreatic disease. Preoperative computed tomography (CT) incidentally showed a huge abdominal cystic lesion of 34x17x25cm (Fig. 1).

Echinoccus serology was negative and the aspiration of the fluid showed normal levels of amylase and no cytological signs of malignancy. A laparoscopic resection was attempted; however, because of lack of exposure due to the large size of the cyst, a conversion to a median laparotomy was necessary. After emptying of the cyst by aspiration of 3 litres of fluid, an “en bloc” resection of the cyst, originating from the mesocolon, was performed (Fig. 2).

Macroscopic specimen showing mesenteric cystic wall following aspiration of the fluid
The postoperative course was uneventful and the patient was discharged at postoperative day 5. Macroscopic examination found a unilocular cyst with fibrotic wall. Microscopically, prominent giant cells and xanthomatous inflammation reaction were present in the wall. Further light brown histiocytes with focal expression of CD31 and D2-40 were found in the specimen (Fig. 3), favouring lymphangioma with cystic-regressive changes.
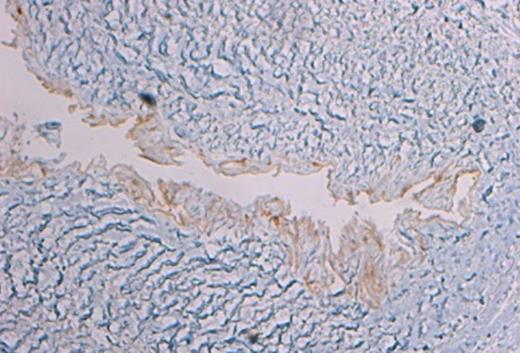
Histology showing immunohistochemistry by marker D2-40 identifying the lymphatic endothelium
No signs of malignancy were found. After a short period of recovery, the required mitral valve reconstruction was successfully performed by a minimal invasive approach. A 1-year follow-up examination including abdominal ultrasonography showed no recurrence.
DISCUSSION
Three types of lymphagniomas are distinguished in the literature: the cavernous lymphangioma, the lymphangioma simplex, and the cystic lymphangioma (1). The cystic form of a lymphagioma was described for the first time in 1828 by Redenbacker (2). Cystic lymphangiomas are very rare and mainly occur during childhood; in 90% of the cases, they are diagnosed before 2 years of age (1,3,4). The estimated incidence of cystic lamphagiomas is approximately one per 20,000 admissions to pediatric hospitals (5,6). Only very few reports exist regarding cystic lymphangioma in adults (7).
Pathogenesis remains unclear. The most accepted theory is based on a lymphatic congestion due to interrupted communication of the draining lymphatic system. However, this does not explain the occurrence of these cystic tumours in the adult population. Therefore, some authors believe that adult manifestations are the result of a delayed proliferation of congenital or acquired lymphoid nests after stimuli such as respiratory infection or local trauma (8). Our patient did indeed have a long history of combat sports.
The clinical presentation of mesenteric lymphatic cysts as described in the present case is variable. Unspecific abdominal symptoms such as pain, distension, nausea and vomiting, diarrhoea, constipation, and weight loss are most common.
Different imaging modalities have been used to diagnose cystic intra-abdominal tumours. Some studies demonstrated ultrasonography as being superior compared with CT regarding the assessment of intracystic structures such as the presence of echogenic contents, a thickness of capsule, and intracystic septation, which may indicate internal bleeding or infection. In cystic lymphangioma, the fluid content is usually described as serous with a density similar to water (Houndfield unit (HU) = 0). Differential diagnosis of intraperitoneal cystic masses includes pancreatic pseudocysts, echinococcal cyst, enteric duplication cysts, cystic mesotheliomas and ascites. Abdominal CT in our patient revealed a density of 18 HU. Ecchinococcus serology was negative as well as the bacteriological and cytological analysis of the aspirated fluid.
Complete surgical resection of lymphangioma remains the treatment of choice in order to reveal symptoms and to prevent recurrences. While aspiration of cystic fluid decreases the size of the cyst for a short time only and has the risk of infection, incomplete excision of lymphangiomas carries a risk of tumour-recurrence ranging from 0-13.6% (9). However, a malignant degeneration was neither seen in the present case, nor described in the literature.
A laparoscopic approach to resect mesenteric cystic lymphangioma has been described in selected cases. In our case, a lack of exposure and impaired visibility caused early conversion to a median laparotomy.
Histological analysis confirmed the total resection of the lesion in our case. Specific immunohistochemical markers for lymphatic endothelial cells have been used such as lymphatic vessel endothelial receptor 1, vascular endothelial growth factor receptor 3, and Prox-1. In addition to CD31, a more recent monoclonal antibody D2-40, specifically binding lymphatic endothelium, was applied by our pathologist (10).
In summary, mesenteric cystic lymphangioma is extremely rare in adults but must be considered as a differential diagnosis of abdominal cystic lesions. Complete surgical resection provides definitive histological diagnosis, and prevents recurrence.



