-
PDF
- Split View
-
Views
-
Cite
Cite
M Dungerwalla, S Loh, P Smart, Adult colonic intussusception: Surgery still the best option, Journal of Surgical Case Reports, Volume 2012, Issue 6, June 2012, Page 3, https://doi.org/10.1093/jscr/2012.6.3
Close - Share Icon Share
Abstract
Intussusception is the telescoping of proximal bowel wall into the lumen of a distal segment. Whilst it is common in children, intussusception in adults is rare, and predominantly occurs secondary to an underlying malignant neoplasm. Abdominal and pelvic computed tomography (CT) is preferred for detection of lead points and lesion localisation.
We present the case of a 79-year-old female with a four-day history of colicky abdominal pain followed by obstipation and distension. CT demonstrated a rounded heterogeneous density protruding into the upper rectal lumen, and also left-sided colonic obstruction. Emergency laparotomy revealed a mid-sigmoid colonic mass intussuscepting into the rectum. Histopathology confirmed a T3N1 moderately differentiated colonic adenocarcinoma.
Given the high likelihood of underlying malignancy, surgical reduction of the intussusceptum may be complicated by perforation and tumour spillage. En bloc resection using oncologic surgical principles remains the first line treatment.
INTRODUCTION
Intussusception is the telescoping of a proximal segment of bowel wall into the lumen of an adjacent, usually distal segment. It is commonly encountered in the small bowel of children, where the aetiology is largely benign and non-operative treatment usually successful (1).
In contrast, intussusception in adults is rare (2). Colonic involvement represents up to 50% of cases, and in 70% the underlying cause is a malignant neoplasm (3). A wide range of other causes in the colon have been described including adenomatous polyps, inflammatory bowel disease, mycobacterial infection, and surgical anastomoses (4).
Presentation is variable in adults, and commonly subacute. Presumably transient asymptomatic radiologic incidentalomas are more frequent, though these are usually seen in the small bowel (5). Those with symptoms report crampy abdominal pain, nausea, vomiting, and occasionally per rectal bleeding. Sigmoidorectal intussusceptions may be associated with diarrhoea and mucus. There may be symptoms of bowel obstruction, especially where the underlying cause is malignant (3). A palpable abdominal mass is infrequent (6).
Accurate clinical diagnosis is difficult. Abdominal and pelvic computed tomography (CT) is the preferred test of choice with the advantage of detection of lead points and accurate localisation of the lesion (3,4). The findings are often pathognomonic and include a sausage shaped soft tissue mass with an eccentric fat density ring contained within, representing mesenteric fat. Mesenteric vasculature is often visible leading into the lesion (7). However increasing bowel wall oedema and progressive vascular compromise lead to a sequence of CT findings dependent on the time course of the intussusception. CT delineation of the underlying aetiology is unreliable, as a neoplastic lead point cannot be distinguished from the mass of an intussusception itself (3).
CASE REPORT
We present the following endoscopic and radiological images to highlight the clinical findings and reiterate the differences in the management of adult and paediatric cases.
A 79-year-old female presented to the emergency department with a four-day history of intermittent, colicky abdominal pain. The patient reported a history of initial non-bloody diarrhoea with mucus, followed by obstipation and distension. Physical examination was consistent with a large bowel obstruction, revealing an uncomfortable patient with a distended abdomen and associated significant left iliac fossa tenderness. The rectum was empty on per rectal examination.
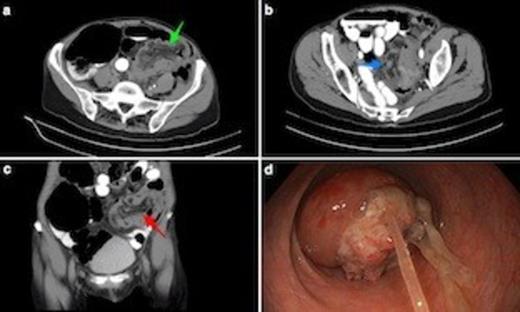
(a) Axial CT scan shows sigmoidorectal intussusception. Note bowel wall thickening. Low attenuation mesenteric tissue is drawn into intussusceptum, with associated caecal dilatation. (b) Axial view through mid-pelvis showing gas between bowel wall of intussusceptum and intussucipiens (i.e. sigmoid colon and rectum: this does not represent intramural gas). (c) Coronal view demonstrating mesenteric vasculature in the intussusceptum. (d) Endoscopic view from mid rectum of tumour intussusception. The underlying lesion was an apple core T3N1 adenocarcinoma of the mid-sigmoid. Note tumour mucus.
Subsequent CT scan revealed a rounded heterogeneous density protruding into the lumen of the upper rectum containing mesenteric fat and blood vessels (Figs. 1a-c). The appearance was suggestive of sigmoidorectal intussusception. There was significant associated proximal large bowel dilatation consistent with left-sided colonic obstruction.
The patient proceeded to emergency surgery. On the operating table, flexible sigmoidoscopy confirmed the diagnosis of intussusception due to a sigmoidal tumour (Fig. 1d). At laparotomy, a mass in the mid sigmoid colon was found with intussusception of the tumour into the rectum. A Hartmann’s procedure was performed. Post-operative recovery was complicated by rapid atrial fibrillation, but was otherwise uneventful. The patient was discharged home nine days after surgery. Histopathology of the surgical specimen showed a T3N1 moderately differentiated colonic adenocarcinoma.
DISCUSSION
This case highlights the key features of management of adult intussusception, and also demonstrates the differences to an approach towards paediatric intussusception. Due to the high rate of malignancy in adults with intussusception, pneumatic or hydrostatic reduction is ill advised given the risk of perforation, which is associated with higher peri-operative mortality and worse prognosis (8,9).
A small number of cases of successful laparoscopic or endoscopic reduction in highly selected patient groups, with known underlying non-malignant aetiology have been reported (10). For the vast majority of presentations however, a malignant cause cannot be excluded. At surgery, reduction of the intussuscepted bowel segment should not be attempted due to the risk of tumour spillage. En bloc resection of the lesion using standard oncologic surgical principles remains the recommended first line treatment for adult colonic intussusception.



