-
PDF
- Split View
-
Views
-
Cite
Cite
BD Stephensen, J Brown, AL Lambrianides, A novel method for managing enterocutaneous fistulae in the open abdomen using a pedicle flap, Journal of Surgical Case Reports, Volume 2012, Issue 6, June 2012, Page 5, https://doi.org/10.1093/jscr/2012.6.5
Close - Share Icon Share
Abstract
A significant proportion of patients with severe intra-abdominal sepsis are managed by leaving the peritoneal cavity open in an attempt to control the infective process, regardless of aetiology. However, a considerable number of these patients develop enterocutaneous fistulae, which compound the clinical situation and delay closure of the peritoneal cavity. We propose a new method of dealing with such fistulae, by simply fashioning a direct pedicle flap to patch the fistulous opening. This method allows control of the fistula and facilitates early closure of the abdomen.
INTRODUCTION
Severe intra-abdominal sepsis is associated with a high morbidity and mortality, and is often managed by leaving the peritoneal cavity open. (1,2) One of the complications arising from this approach is the development of enteric fistulae. This occurs in approximately twenty-five percent of patients, and is associated with a mortality of forty-two percent. (3) Management of these fistulae in the setting of sepsis and malnutrition poses a significant surgical challenge. We report a novel method in the management of such a fistula with a pedicle flap, which was successful after a single attempt in a single patient, and thus allowed staged closure of the abdominal wall defect.
CASE PRESENTATION
A fifty-seven year old morbidly obese male patient presented with small bowel obstruction secondary to massive irreducible incisional hernia following midline laparotomy and anterior resection for Dukes C rectal cancer ten years earlier. In view of significant comorbidities, and in the absence of clinical strangulation, he was managed conservatively in the intensive care unit. He was discharged to the ward when bowel function appeared to have returned, where he subsequently developed rapidly progressive cellulitis over the hernia (Fig. 1).

Massive incisional hernia with necrotising fasciitis of the overlying soft tissues

Necrotic small bowel with perforation and faecal contamination within hernial sac
At laparotomy, a long segment of necrotic distal small bowel with multiple perforations and free faecal contamination was identified within the hernia sac, with necrotising fasciitis of the overlying abdominal wall (Fig. 2). Necrotic tissue was debrided, resulting in complete excision of the skin, subcutaneous tissue and muscle layers of the anterior and lateral abdominal wall. The necrotic small bowel was resected and primarily anastomosed (Fig. 3). The patient was managed in intensive care with daily dressings and further debridement of necrotic tissue when required, with eventual control of his sepsis. The abdominal cavity was closed with Bard Composix™ EX mesh, but this was subsequently removed due to ongoing infection. The wound was allowed to granulate.

After debridement of necrotic abdominal wall and small bowel resection
Frequent dressings and prolonged exposure resulted in deserosalisation of the small bowel with fistula formation. After computed tomography examination and small bowel follow-through to exclude sepsis and distal obstruction, this was initially managed conservatively with total parenteral nutrition to afford bowel rest, daily wound care and octreotide. Ongoing failure of conservative measures prompted attempts to close the fistula using a fibrin sealant (3), with no success. Subsequent closure attempts with Algisite™ M (Smith and Nephew) patches impregnated with cyanoacrylates were also unsuccessful.
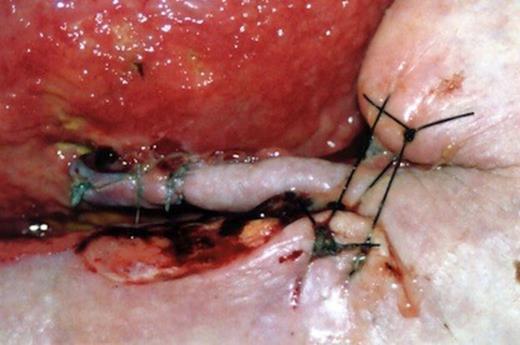
Closure of the fistulous opening was eventually achieved by means of interrupted absorbable sutures, which transfixed the entire thickness of the bowel wall. The central suture crossing the fistula opening was inserted last so that the tension, having been taken up by more distantly placed sutures, was less likely to cut through the oedematous bowel wall. The sutures were inserted in the long axis to avoid narrowing of the lumen. The closure was reinforced by means of a direct viable pedicle flap fashioned from adjacent healthy tissue, held in place by tying the long ends of the primary sutures over the flap (Fig. 4). Only when the flap was soundly incorporated into the defect and had developed a new blood supply was the pedicle divided. In our case, this was performed after two weeks.

The pedicle flap successfully controlled the fistula, with no subsequent leak following the repair. The wound was then closed in a staged fashion using flaps. The patient was discharged home with an intact abdominal wall, and remains well at follow up (Fig. 5).
DISCUSSION
Managing the open abdomen remains challenging. Few options exist for closing the defect and treating subsequent complications. Enteric fistulae may occur in up to twenty-five percent of patients managed with an open abdomen. (5) Fistulae develop in the open abdomen due to local intestinal necrosis as a result of exposure to the environment, debridement from repeated dressing changes or anastomotic dehiscence. (2,3) Application of a stomal appliance to divert the fistula output is impossible due to the absence of surrounding skin. (4) In the presence of constant contamination, the rate of spontaneous closure of the fistula is greatly reduced, and skin disruption may worsen. Many techniques for fistula management have been trialed with limited success, and often conservative management with bowel rest and parenteral nutrition fails. Traditional surgical techniques with resection of the affected segment of bowel with primary anastomosis are often technically impossible because of bowel oedema, a foreshortened mesentery and a non-compliant abdominal wall. (5) Indeed, further bowel resection may be precluded by previous extensive bowel resection, as in our case.
The use of an acellular dermal matrix as a biologic patch and fibrin glue was reported as a successful technique in treating enteric fistula in one patient, and preventing fistula formation in a further two patients with deserosalisation of the small bowel. (3) Fibrin sealant alone has been used successfully on enterocutaneous and enteroenteral fistulae. (6,7). Our experience with fibrin glue did not mirror this success.
Another option exists in excising the mass of granulated bowel and fistula using a lateral incision. Bowel continuity can be reestablished and the abdominal wall defect closed with mesh, (5) but this procedure is often technically precluded. Alternatively, simple skin grafting of the granulation tissue around the fistula allows eventual application of a stomal appliance, but the patient then requires definitive surgery for closure of the defect and fistula at a later stage. (4)
Our technique allows early closure of the fistula, which permits definitive treatment of the defect without significant delay and without concerns regarding contamination. We advocate the consideration of this technique initially, if conservative measures have failed and factors that would adversely affect closure, such as distal obstruction, sepsis and malignancy, have been excluded, although our experience is limited. It is inexpensive, technically simple, and has the benefit of utilising healthy, well-vascularised autologous tissue.



