-
PDF
- Split View
-
Views
-
Cite
Cite
T E Locke, D Stewart, K Patel, A Takou, Small bowel ischaemia and perforation as a complication of Henoch-Schönlein Purpura in a previously healthy adult, Journal of Surgical Case Reports, Volume 2012, Issue 4, April 2012, Page 9, https://doi.org/10.1093/jscr/2012.4.9
Close - Share Icon Share
Abstract
Henoch-Schönlein purpura is a small vessel vasculitis with multi-system manifestations that commonly affects children. We describe a case of new onset Henoch-Schönlein purpura in a previously healthy 42-year-old female who required an emergency laparotomy for small bowel perforation.
INTRODUCTION
Henoch-Schönlein purpura (HSP) is a small vessel leukocytoclastic vasculitis that typically presents in childhood. The incidence has been estimated at 10 cases per 100,000 children per year, with a slight male preponderance (1). The condition is believed to be triggered by exposure to an unknown antigen with subsequent vascular deposition of IgA containing immune complexes. Multi-system manifestations have been described, most commonly affecting the skin, joints, and renal and gastrointestinal system. The condition is commonly self-limiting and management usually entails symptomatic treatment and the use of immunosuppressive therapy.
Although there is a wealth of discussion relating to paediatric HSP, there is little equivalent consideration regarding the adult form of the disease. Furthermore, there is limited discussion relating to intestinal manifestations of adult onset HSP. It is on this basis that we describe a case of small bowel ischaemia and perforation in a 42-year-old adult with previously undiagnosed HSP.
CASE REPORT
A previously healthy 42-year-old female was referred to a dermatology clinic with a few days history of painless non-blanching papular lesions on her legs (figure 1), swollen hands and generalised myalgia. An infection screen (including hepatitis serology and anti-streptolysin O titre), immunology screen and skin biopsy was performed and the patient was given a weeklong course of oral prednisolone at a dose of 15 mg once daily.

A week later the patient required emergency admission with a three day history of generalised abdominal pain and vomiting. An initial abdominal radiograph was suggestive of small bowel obstruction. However, computerised tomography revealed extensive small bowel wall thickening and ascites without evidence of mechanical obstruction or viscus perforation (figure 2). In addition, the C-reactive protein (CRP) and urea were elevated with a raised urine protein/creatinine ratio suggestive of nephritis. Overnight the patient deteriorated rapidly developing peritonitis and septic shock. Following a bolus dose of intravenous methylprednisolone, an emergency laparotomy revealed turbid ascites and patchy ischaemia throughout the entire small bowel with a perforation 150 centimetres from the duodenojejunal flexure. The perforated segment was excised and a defunctioning ileostomy and mucous fistula was formed. Post-operatively, the patient was admitted to the intensive care unit for multi-organ support and commenced on a course of intravenous methylprednisolone with two cycles of intravenous cyclophosphamide.

On the tenth post-operative day, she became suddenly unresponsive due to a bradyarrhythmia that progressed to asystole. Following a brief period of cardiopulmonary resuscitation during which cardiac output was restored, a temporary pacing wire was placed to prevent further dysrhythmias. Subsequent echocardiography and biochemistry excluded any significant myocarditis.
The histopathology report for the skin biopsy showed severe acute necrotising leukocytoclastic vasculitis affecting small and medium-sized vessels. The infection and immunology screening tests were negative, in particular IgA was not detected on immunofluorescence. Histological analysis of the small bowel segment revealed the presence of a small vessel vasculitis with typical fibrinoid necrosis suggestive of HSP (figure 3).
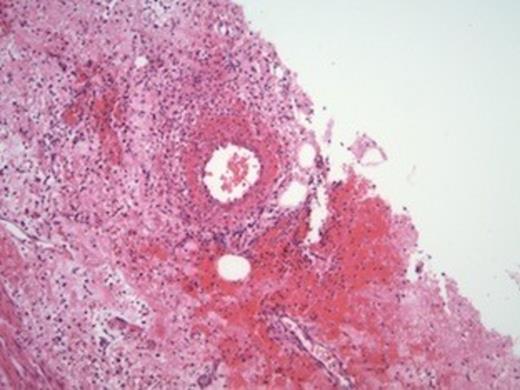
A small-sized artery displaying inflammation of the wall and focally fibrinoid necrosis.
Over the next two weeks the patient made steady progress towards recovery, although this was complicated by the formation of a large pelvic abscess, identified on computed tomography, which required the insertion of a percutaneous drain. Just over one month after her initial presentation, the patient was discharged from hospital but continues on oral steroids and intravenous cyclophosphamide. At initial follow up, her clinical status and laboratory findings (CRP, urea and urine protein/creatinine ratio) had all significantly improved. In due time, a reversal of her ileostomy will be considered.
DISCUSSION
HSP can present at any age, however, it is typically a disease of childhood. The majority of patients are younger than ten years old and there is little epidemiological data relating to adolescence and adulthood. Common clinical manifestations include a purpuric rash, abdominal pain, arthralgia/arthritis and renal disease. The gastrointestinal manifestations of HSP are more commonly described in children and reports suggest that adults rarely require surgical intervention (2).
Although IgA complexes were not identified in the skin biopsy in this report, the histopathological assessment of the small bowel revealed features highly suggestive of a diagnosis of HSP. In addition, the clinical findings in this case satisfy the diagnostic criteria suggested by the American College of Rheumatology and the European League Against Rheumatism (see figure 4) (3). Indeed, a recent study from Massachusetts General Hospital highlights a subset of HSP cases with no evidence of vascular IgA deposition in the skin (3).
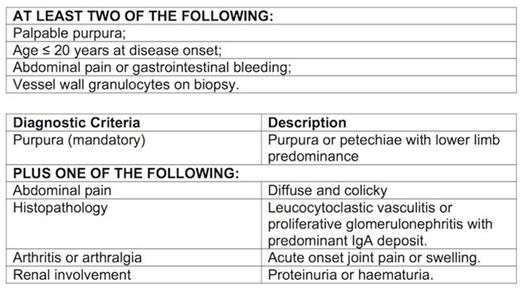
American College of Rheumatology (top) and the European League Against Rheumatism Diagnostic Criteria (bottom) of HSP.
We only identified six similar English language case reports (describing seven patients) in the medical literature (4-9). Five patients were male and although only four displayed gastrointestinal features at initial presentation, six patients required surgical intervention. Five patients were given steroid therapy; of which three began this treatment before the onset of an acute abdominal picture, which is identical to our presented scenario. Outcomes were not always positive (three patients died), although one case was complicated by cardiac and renal involvement and gastrointestinal disease was only diagnosed at post-mortem (8).
Although a recognised risk factor for gastro-intestinal bleeding and perforation, steroid therapy early in the course of an episode of HSP has been shown to be beneficial in preventing extra-renal symptoms (10). In our case report, steroid therapy was commenced a week before the patient developed abdominal symptoms. Similar findings have been described previously (5,6,9). It is impossible to be certain about the role of oral steroids in the small bowel perforation in this case, but it would appear unlikely that glucocorticoid therapy would be responsible for patchy small bowel ischaemia. The authors consider the intra-operative findings more likely representative of a global pathological process attributable to HSP vasculitis.
Despite HSP typically following a benign self-limiting course, gastrointestinal manifestations can be rapidly fatal. This report demonstrates the importance of considering systemic vasculitides such as HSP in the differential diagnosis of adults presenting with acute abdominal symptoms with preceding symptoms and signs that may indicate an underlying vasculitic process. Furthermore, early surgical intervention has the potential to reduce morbidity and mortality.



