-
PDF
- Split View
-
Views
-
Cite
Cite
M Abdulmajed, A Ghalib, M Mohamed, P Marsh, Intestinal metastasis from primary epidermoid anal carcinoma in a 34 year old male presented with acute bowel obstruction, Journal of Surgical Case Reports, Volume 2012, Issue 2, February 2012, Page 1, https://doi.org/10.1093/jscr/2012.2.1
Close - Share Icon Share
Abstract
Squamous cell carcinoma (SCC) of the anal canal is a rare condition comprising only 2–4% of all cancers of the colon, rectum and anus. The most common sites of metastases are liver and lung.
We report a case of 34-year-old male, who presented with diarrhoeal illness and an acutely tender protruding anal lesion initially thought to be thrombosed external hemorrhoid. Examination under anaesthesia revealed a hard and fixed mass at the level of dentate line, which was biopsied. On histopathological examination, it was confirmed as primary moderately differentiated keratinising squamous cell carcinoma. Despite initial response to concomitant chemo-radiation, 4 months later, the patient presented with large bowel obstruction. On laparotomy, a large mass involving the terminal ileum and caecum was identified. Histopathological examination revealed metastatic spread from primary anal lesion. To the best of our knowledge, this is the first reported case of a squamous cell carcinoma of anus with bowel metastasis.
INTRODUCTION
Anal tumours are uncommon tumours of the gastrointestinal tract that constitute only 5% of anorectal malignancies with the peak incidence seen during the seventh decade of life. (1) Nearly 80% of anal canal tumours are squamous cell carcinomas (SCC). Anal cancer is primarily a loco-regional disease, which rarely (<10% of cases) metastasises. (2) Most common sites of extra-pelvic metastases from squamous cell cancer of anal canal are the liver, lungs and extra-pelvic lymph nodes, although spread to peritoneum, bone and other sites may also occur. (3) We herein report an unusual case of SCC of anus with small and large bowel metastases in a young male presented with large intestinal obstruction four months after the primary diagnosis.
CASE REPORT
A 34-year-old white heterosexual male presented with a 3-week history of diarrhoeal illness and an acutely tender protruding anal lesion after evacuation thought to be a thrombosed external hemorrhoid at left lateral position on initial examination.
Examination under general anaesthesia revealed a hard and fixed mass at the level of dentate line protruding down into anal canal and two peri-anal abscesses along with bilateral palpable inguinal lymphadenopathy. Incision and drainage of the abscesses was performed and biopsy was taken from anal lesion and anal verge. Histopathological analysis revealed primary moderately differentiated keratinising SCC with no evidence of vascular invasion.
Staging MRI scan showed large tumour protruding through anal canal involving left levator ani muscle and left seminal vesicle and enlarged bilateral pelvic lymph nodes with no evidence of liver metastasis. Subsequently, de-functioning colostomy was done and patient received chemotherapy with an initial cycle of Cisplatin and Fluorouracil, followed by combination of Fluorouracil, Mitomycin and radiotherapy. His tumour responded well and showed considerable reduction in size on subsequent imaging.
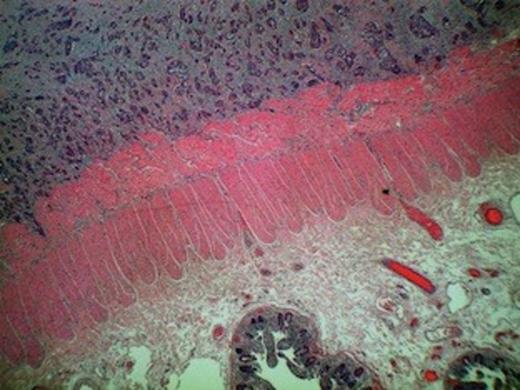
Squamous cell carcinoma metastasis infiltrating peritoneal fat and serosa evident of right hemicolectomy specimen
Despite an initial response to treatment, four months later, the patient presented with clinical picture suggestive of large bowel obstruction. An explorative laparotomy unveiled a large mass involving the terminal ileum and caecum along with dense adhesions of ileocaecal loops. A 4 cm nodule in the right lobe of liver was also discovered. The patient underwent right hemicolectomy with an end-to-end ileocolic anastomosis. The surgical specimen consisted of 21 and 15 cm length of small and large bowel, respectively. The central 10 cm of the bowel was of undeterminable nature due to its tortuous nature caused by innumerable adhesions. The mucosa was unremarkable except for focal oedema. Histological examination showed poorly-differentiated squamous cell carcinoma infiltrating serosa with prominent intravascular spread. The tumour was predominantly confined to the peritoneal fat and serosa with no obvious invasion of the muscularis, submucosal, and mucosal layers (Figure 1 and 2). The appearance was consistent with metastatic spread from primary anal lesion. Unfortunately, the patient did not recover and died from multiple organ failure on the fourth post-operative day.
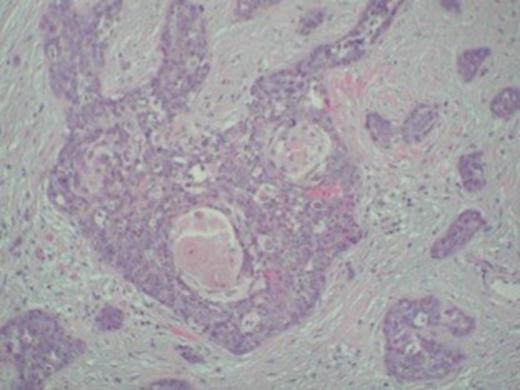
Keratin pearls confirming squamous cell carcinoma metastasis in the tumour specimen
DISCUSSION
Metastatic tumours to the large bowel are rare and can pose diagnostic and management difficulties. In small bowel, metastatic tumours outnumber the primary tumours but it is rarely involved by metastasis from a tumour originating outside the peritoneal cavity. (4)
The malignancies, known to cause secondary deposits in large bowel, are stomach, breast, ovary, kidney, bladder, prostate, lung, cervix, and melanoma. (4) The common primary tumours that metastasise to small bowel are carcinoma of lung, cervix uteri, melanoma, other parts of the gastro-intestinal tract (stomach and colon), and kidney. (5,6) In the present case, the metastasis was from a moderately-differentiated SCC of the anus which has never been reported in the literature. The possibility of a primary SCC of the bowel was excluded since the tumour was located in serosa with no evidence of dysplasia or atypia in intestinal epithelium and staging MRI did not show any evidence of primary bowel tumour.
The route of metastasis to the ileum depends upon the site of the primary lesion. The different mechanisms postulated for small bowel metastasis from abdomen or pelvis include; retrograde lymphatic spread following initial blockade of para-aortic or mediastinal lymph nodes, peritoneal seedlings, direct extension by continuity or by permeation of the lymphatic spaces in connective tissues and haematogenous route. (7) In our case, haematogenous route appeared to be the most likely mode of spread due to the presence of liver metastasis and wide spread vascular invasion on histopathology.
The most common presenting clinical picture of metastatic small bowel tumour is that of partial or complete small bowel obstruction. Less often, the patient may present with perforation of the bowel or haemorrhage from the lesion. The causes of malignant bowel obstruction include extrinsic or intrinsic occlusion of the lumen and intestinal motility disorders. (8) In this case, malignant bowel obstruction can be explained by the extensive adhesions in the intestinal wall seen intra-operatively and caused by metastasis.
Even though management of metastatic tumor to bowel is only palliative, considerable relief can be obtained by resection of obstructed bowel and therefore, in the absence of overwhelming systemic disease, surgical intervention is still an option. (9) Karanikas et al, (10) in their study on 31 patients with metastases to large bowel concluded that clinically-evident metastases to large bowel confer a poor prognosis but surgical resection can, in selected patients, produce a worthwhile survival.
To sum up, our case report reveals the possibility of intestinal obstruction caused by metastasis from primary SCC of the anus, a scenario which has not been published in the literature before.



