-
PDF
- Split View
-
Views
-
Cite
Cite
Robert Nash, Anooj Majithia, Atheer Ujam, Arvind Singh, Ossicular malposition in Larsen syndrome: a case report, Journal of Surgical Case Reports, Volume 2012, Issue 11, November 2012, rjs007, https://doi.org/10.1093/jscr/rjs007
Close - Share Icon Share
Abstract
Larsen syndrome is a rare condition that causes multiple large joint dislocations and characteristic flattened facies. We present a case of a patient with Larsen syndrome with a conductive hearing loss due to ossicular malposition/dislocation. We discuss the aetiopathogenesis of hearing loss in Larsen syndrome.
INTRODUCTION
Larsen syndrome is a rare congenital disorder characterized by multiple large joint dislocations and flattened facies. It was originally described in 1950 [1], and occurs in ∼1:100 000 live births. In addition to sporadic cases, both autosomal dominant and autosomal recessive patterns of inheritance are recognized.
Genes that have been implicated in Larsen syndrome include filamin B [2], which is involved in the cytoskeletal architecture, and carbohydrate sulphotransferase 3, which has also been implicated in other skeletal dysplasias [3].
Larsen syndrome has been associated with a number of other anomalies, many of which have relevance to the otolaryngologist. These include cleft palate, orofacial malformations, atlanto-axial subluxation, subglottic stenosis and tracheomalacia [4].
We present a case of Larsen syndrome being associated with ossicular malposition causing a conductive hearing loss.
CASE REPORT
A 7-year-old female presented with a longstanding history of bilateral hearing loss, more noticeable on the right side. She had a recent diagnosis of Larsen syndrome, and was homozygous for the CHST3 gene, for which the inheritance is autosomal recessive. She did not have a filamin B mutation.
There was no evidence of facial dysmorphia, although she had skeletal dysplasia and congenital right-sided hip and knee dislocations. Furthermore, she had previous left hip and knee subluxations, and hallux valgus. Prior echocardiography had revealed thickened aortic valve cusps.
On examination, she was noted to have narrow ear canals, with grade 1 microtia. She had bilateral middle ear effusions in keeping with glue ear. After a period of active surveillance, her glue ear resolved, but she continued to have a hearing deficit, with a right-sided mild conductive hearing loss with thresholds of ∼40 dB.
At this stage, a computed tomography (CT) scan of the temporal bone was undertaken. The stapes was maloriented on the oval window; however, the other ossicles appeared normal (see Figs 1 and 2). There was no middle ear effusion at the time of the CT scan.
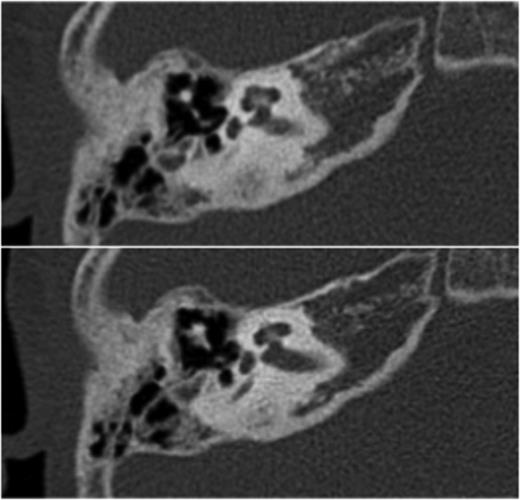
Transverse high-resolution CT demonstrates intact ossicles with malposition of the stapes
After discussions regarding the options for management, she was managed conservatively. She did not require hearing aids.
DISCUSSION
There have been a handful of previous reports of an association between Larsen syndrome and hearing loss. Both conductive and sensorineural hearing deficits have been reported [5]. In those patients with conductive hearing loss, an ossicular abnormality has been shown on only three occasions [6]. On each of these occasions, there was dysplasia of either the incus or the incostapedial joint (ISJ). All of these cases also report fixation of the stapes footplate, and tympanometry reveals stiffening of the ossicular chain. Stapedial reflexes are absent [7].
In this case, the conductive hearing deficit occurs despite a normal incus and ISJ. This indicates the importance of the articulation of the stapes on the oval window in the pathogenesis of the hearing loss in these cases. Furthermore, this case also demonstrates an element of commonality with the aetiopathogenesis of otosclerosis, in which the overgrowth of bone in the otic capsule also causes failure of articulation of the stapes in the oval window. Due to the delicate bony formation of the middle ear, the conductive component of hearing may be affected by a number of genetic bone disorders. In addition to Larsen syndrome and otosclerosis, osteogenesis imperfecta and Paget's disease are frequently associated with hearing loss.
Very little is known about the management of these patients. There is one case in which stapedotomy has been shown to notably improve hearing in a 12-year-old [8]. However, management generally depends on the use of hearing aids [9], and the treatment of frequent and recurrent middle ear effusions [10].
In conclusion, we present a case of conductive hearing loss in a patient with Larsen syndrome. The hearing loss is due to malposition of the stapes on the oval window. When present, genetic bone disorders frequently affect both the conductive and sensorineural hearing systems.



