-
PDF
- Split View
-
Views
-
Cite
Cite
Antonio Privitera, Eric J Dozois, A novel approach to management of a sacral defect in ileal pouch-sacral fistula, Journal of Surgical Case Reports, Volume 2012, Issue 11, November 2012, rjs006, https://doi.org/10.1093/jscr/rjs006
Close - Share Icon Share
Abstract
Fistula formation after restorative proctocolectomy poses a challenge to the surgeon and sometimes can lead to the excision of the pouch. While pouch-vaginal fistulas are more common, pouch-sacral fistulas are a rare event and treatment is still controversial. The authors report a case of pouch-sacral fistula which was treated successfully with a novel approach comprising pouch revision, debridement of sacrum and placement of a human acellular dermal matrix (Alloderm) mesh to patch the residual large sacral defect. This is the first report of the use of Alloderm under this rare condition.
INTRODUCTION
Restorative proctocolectomy with ileal pouch-anal anastomosis has become a standard procedure for patients with familial adenomatous polyposis (FAP) and chronic ulcerative colitis. A good long-term pouch function is to be expected in >90% of patients [1]. Pelvic sepsis following this procedure has been reported in up to 25% of cases and has been shown to have a negative impact on pouch function and late failure rate [1, 2]. The incidence of pouch-related fistula is reported in 4–16% of cases with the most common being pouch-vaginal [3, 4]. On the other hand, pouch-sacral fistula is a rare event [1, 5, 6]. Treatment of a pouch-sacral fistula includes pouch revision and curettage of the sacrum. We describe the use of a human acellular dermal matrix (Alloderm) mesh to patch a large sacral defect in conjunction with pouch revision.
CASE REPORT
A 20-year-old man was admitted with pelvic and hip pain, anorexia and loss of weight. His past surgical history revealed a proctocolectomy with ileo-pouch anal anastomosis for familial adenomatous polyposis (FAP) carried out in another institution 3 years previously. This had been complicated by an anastomotic leak treated with a loop ileostomy that was taken down 6 months later. Subsequently, he developed a new pelvic collection and persistent pouch-presacral space fistula that was treated with a laparoscopic drainage and repeat loop ileostomy. A follow-up magnetic resonance imaging (MRI) showed improvement but persistence of pelvic phlegmon. Cultures of presacral fluid revealed a polymicrobial flora including Escherichia Coli, Enterococcus, Bacillus species and Eikenella Corrodens.
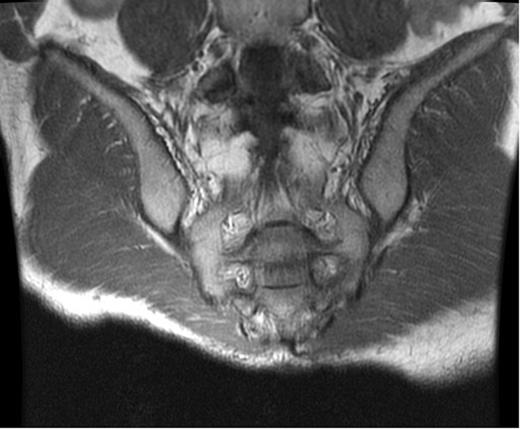
At the time of evaluation at our institution, he was afebrile and the laboratory tests, including inflammatory markers, were unremarkable. A computed tomography (CT) scan of the abdomen and pelvis showed a presacral fluid collection with a fistula between the pouch and the sacrum (Fig. 1). An MRI of the pelvis was performed and this revealed signs of osteomyelitis involving the S2–S4 vertebrae (Fig. 2). A laparotomy was performed and the ileal-anal pouch anastomosis was taken down, the sacrum was debrided leaving a large anterior bony defect. No omentum was available, so a 10 cm × 10 cm piece of Alloderm was used to cover the defect. The pouch fistula was excised and closed and the revised pouch re-anastomosed to the anus. The patient made an uneventful recovery and was discharged on the seventh postoperative day. Cultures from the sacral debrided tissue yielded Actinomyces spp. and a 12-week course of antibiotics (clindamycin) was commenced.
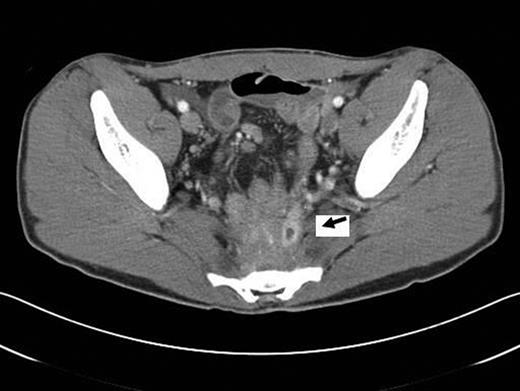
CT scan. Presacral air-fluid collection with a pouch-sacral fistula (arrow).
DISCUSSION
Sacral osteomyelitis following pouch surgery is usually the result of chronic pelvic sepsis. CT and MRI show local oedema with associated cortical destruction and periosteal reaction. Nuclear scans are often non-specific and do not provide adequate details to guide resection margins. CT-guided aspiration and culture of pelvic collections are helpful to guide antibiotic treatment [7]. Although percutaneous drainage may offer a temporizing approach, it is not a definitive therapy for cases of suspected osteomyelitis [8]. The most successful treatment involves aggressive surgical debridement, removal of the offending agent, long-term antibiotics and dead-space management [9].
The development of a fistulous tract between the pouch and the sacrum is rarely reported. Taylor et al. reported four cases of pouch-sacral fistula [1]. Three patients were treated with fistula division, debridement and diverting loop ileostomy. The sacral defect was covered with omentum. Two maintained normal pouch function, while one patient remained defunctioned. One patient underwent pouch excision in another institution and presented with pelvic sepsis associated with sacral and L5 vertebral destruction that required bony resection and decompression. Bursics et al. reported a case where the fistula originated from the efferent blind loop of the pouch. Excision of the fistula was carried out and the pouch defect was sutured. The sacrum was debrided and a gentamycin sponge was left in the cavity [5]. In our case, pelvic sepsis was likely exacerbated by actinomycosis that is known to cause chronic infection that is difficult to treat. The sacral defect was covered with Alloderm that has been shown to be a suitable material following sacral resection [10]. In fact, it has similar tensile strength to polypropylene, and it is non-allergenic and possibly less likely than the synthetic mesh to cause inflammation leading to small bowel adherence.
We believe that part of our patient's successful outcome was due to our ability to separate the inflamed sacral defect from the revised pouch. We believe that it is a valuable alternative when the omentum is not available.
Conflict of interest
None declared.



