-
PDF
- Split View
-
Views
-
Cite
Cite
RJ Heitmann, RO Burney, Endometrial appearance in the presence of communicating hydrosalpinx, Journal of Surgical Case Reports, Volume 2012, Issue 1, January 2012, Page 8, https://doi.org/10.1093/jscr/2012.1.8
Close - Share Icon Share
Abstract
We report the hysteroscopic findings in a 22 year old nulligravid patient with bilateral communicating hydrosalpinges. The inflamed hyperemic endometrial cavity encountered preoperatively normalized at second look hysteroscopy six months after bilateral tubal interruption. The patient underwent successful IVF with culmination in a singleton, live birth. We propose that an inflamed appearance at hysteroscopy, done for endometrial cavity screening, should prompt a dedicated study to rule out hydrosalpinx prior to proceeding with IVF treatment. To date, such a hysteroscopic endometrial phenotype in the presence of hydrosalpinx has not been well characterized.
INTRODUCTION
The deleterious impact of hydrosalpinx on fertility is best exemplified by studies showing a 50% reduction in IVF pregnancy rates in their presence (1). Chlamydia infection and pelvic inflammatory disease are associated with an increased risk of both tubal infertility and ectopic pregnancy, with the association proportionate to the number of infections(2).
Various theories have been proposed to explain the observation of lower IVF pregnancy rates in the setting of hydrosalpinx, to include mechanical effects, embryo and gametotoxicity, decreased expression of key implantation molecules, and/or a direct effect on the endometrium leading to intrauterine fluid formation(3). Drainage of hydrosalpingeal fluid into the endometrial cavity may exert a mechanical effect by washing the transferred embryo from the cavity. Cultured epithelial cells isolated from hydrosalpinx affected tubes produce a fluid which is hostile to both spermatozoa and early mouse embryo development(4).
Multiple studies have demonstrated deficiency in endometrial markers of embryo receptivity in the presence of hydrosalpinx. IL-2, T lymphocytes, CD3+, CD8+, CD4+, alpha V Beta 3 integrin, LIF, MMPs and HOXA10 have all been shown to be decreased in the endometrium from women with versus without hydrosalpinx(5-8) Though molecular inflammatory changes in the setting of hydrosalpinx are documented, a hysteroscopic endometrial phenotype in the presence of hydrosalpinx has not been well characterized.
CASE REPORT
A 22-year old nulligravida presented with a history of primary infertility. Eighteen months prior to presentation, she was diagnosed with a chlamydial infection by cervical culture and treated with a single dose Azithromycin. A negative Chlamydia culture was confirmed four months prior to presentation. As part of her initial infertility evaluation at our center, a hysterosalpingogram (HSG) was performed in a window of Doxycycline prophylaxis which demonstrated bilateral hydrosalpinges, with the right tubal diameter measuring greater than the left and bilateral tubal occlusion (Figure 1).
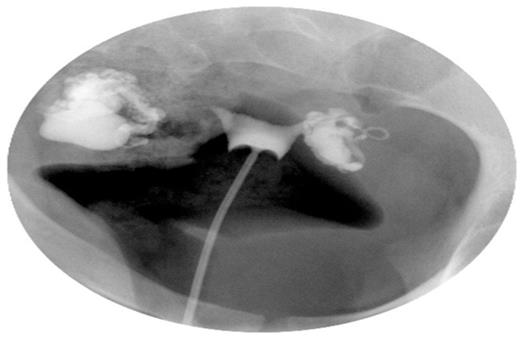
Hysterosalpingogram demonstrating bilateral distal tubal occlusion with hydrosalpinges
Staged combined endoscopy was performed in the operating room. Hysteroscopy revealed endometrial inflammation as evidenced by diffuse hyperemia and mucosal oedema (Figure 2A). Laparoscopic findings were significant for a right sided hydrosalpinx measuring over 2 centimeters in diameter and dense adhesions of the bowel to the left hydrosalpinx and ovary. Chromopertubation confirmed bilateral distal tubal occlusion. She underwent right salpingectomy and left tubal occlusion at the visible isthmic region via clip placement. Histopathology of the salpingectomy specimen revealed chronic inflammation. She experienced an unremarkable postoperative course and was scheduled for in vitro fertilization (IVF) treatment.
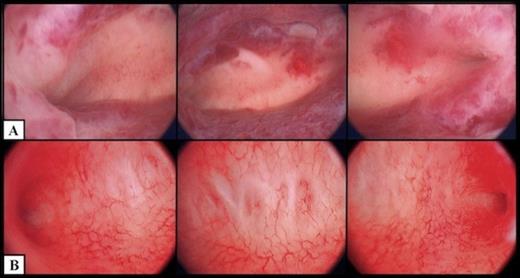
Hysteroscopic appearance of endometrial cavity immediately pre-salpingectomy (A) and six months after interruption of communication with hydrosalpinges (B). For each series, images from left to right depict right cornual, fundal and left cornual regions, respectively.
Six months later, the patient underwent hysteroscopic endometrial cavity evaluation in preparation for IVF. At hysteroscopy, a normal endometrium was visualized (Figure 2B). Specifically, the previously seen hyperemia and stromal oedema had resolved. The patient subsequently underwent IVF with transfer of a single blastocyst culminating in the delivery of a healthy infant at term.
Discussion
Given the importance of tubal patency in non-IVF treatment and the detrimental impact of tubal pathology such as hydrosalpinx, oviductal evaluation represents an important part of the initial female infertility work up. Typically, hydrosalpinges have been detected via hysterosalpingogram or laparoscopy. Given the trend among women to present for infertility care later in the reproductive lifespan, patients undergoing IVF may not have had prior tubal evaluation via either of the standard modalities. Transvaginal ultrasound in the detection of hydrosalpinx has been reported, albeit with user-dependent sensitivity. Office hysteroscopy is an increasingly used technique for endometrial cavity evaluation prior to IVF. The present case suggests that an inflamed endometrial appearance may be a hysteroscopic sign of a communicating hydrosalpinx requiring dedicated tubal study prior to initiating fertility treatment
As depicted in Figure 2, the endometrial surface appears erythematous with friable and tortuous vascularity in the setting of a hydrosalpinx, and normal appearing after surgical interruption of hydrosalpingeal drainage. Subsequent IVF treatment and transfer of a single blastocyst resulted in an intrauterine pregnancy, with subsequent term delivery, indicative of functional embryo receptivity on a molecular level, although no molecular evidence is available for confirmation.
In view of these findings, we propose an inflamed appearance at hysteroscopy for endometrial cavity screening should prompt a dedicated study to rule out hydrosalpinx prior to proceeding with IVF treatment. To date, such a hysteroscopic endometrial phenotype in the presence of hydrosalpinx has not been described.



