-
PDF
- Split View
-
Views
-
Cite
Cite
D Mendis, N Molony, ‘Coughing up a tonsil’ – oesophageal leiomyoma, Journal of Surgical Case Reports, Volume 2012, Issue 1, January 2012, Page 3, https://doi.org/10.1093/jscr/2012.1.3
Close - Share Icon Share
Abstract
We report on a case of oesophageal leiomyoma presenting as a potential cause of sudden airway obstruction. The patient presented with a large mass in the oral cavity after an episode of forceful vomiting. The operative findings and histology of which confirmed this to be an oesophageal leiomyoma emanating from the upper oesophagus, a rare finding. The mass was excised and the patient’s subsequent post-operative recovery and follow-up has been unremarkable.
This diagnosis should be borne in mind when one is referred the odd–sounding case of a patient who appears to have ‘coughed up their tonsil’.
INTRODUCTION
Benign tumours, such as leiomyomas account for less than 1% of all hypopharyngeal and oesophageal tumours (1,2). Leiomyoma is the most common benign oesophageal neoplasm, the reported post-mortem incidences range from 0.005% to 5.1%. However in comparison to oesophageal carcinoma they are relatively rare. Usually presenting in the 3rd-5th decade with a male:female ratio of 2:1 (3).
CASE REPORT
We report on a 48-year old female ex-smoker who presented to the Emergency department with a sizeable right-sided oral cavity mass associated with audible stertor, but no significant airway compromise in the upright position. The mass appeared after an episode of forceful vomiting having had a cough for two weeks. The remainder of the history was unremarkable apart from an alcohol intake of up to 27 units of wine a week.
Flexible nasoendoscopy suggested an epithelial attachment of the mass to the right tonsil. The patient subsequently underwent a general anaesthetic examination with possible tonsillectomy. This demonstrated that the large pedunculated necrotic mass was in fact, appearing to arise from the right piriform fossa and not the tonsil confirmed by rigid pharyngolaryngo-upper oesophagoscopy. The upper oesophagoscopy was limited to 20 centimetres (cm) due to mucosal oedema. The mass was ligated at its base (silk suture) and sent for further analysis (figure 1). It is likely that the mass had acutely twisted and protruded into the upper oesophagus causing obstructive symptoms leading to the history of sudden-onset vomiting. The patient’s post-operative recovery was uneventful and an outpatient review was arranged.
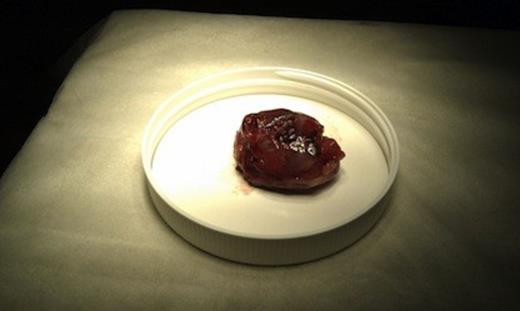
Histology confirmed a benign leiomyoma macroscopically measuring 5 x 3.5 x 3cm, which had been shelled out of a squamous covering with no evidence of dysplastic or malignant change. Further imaging [computerised tomography (CT) of neck] demonstrated a remnant of the base of the lesion low in the piriform fossa possibly going up to the upper oesophagus and a barium swallow revealed some oesophageal mucosal irregularity at approximately 21cm.
Further flexible nasoendoscopy assessment in clinic was concerning and unhelpful in assessing the piriform fossa (right side – erythematous and oedematous), prompting a further general anaesthetic rigid laryngopharyngo-upper oesophagoscopy procedure to exclude a synchronous tumour. This revealed a normal piriform fossae and a stump in the left posterior upper oesophagus at approximately 19cm, with the original silk suture attached to it suggesting that the mass was in fact an oesophageal leiomyoma. Biopsies of the stump confirmed oesophageal mucosa only.
The patient was kept under close review jointly with the general surgeons for flexible oesophageal endoscopy and eventually underwent a flexible endoscopy whereby the stump was removed, confirming the same histology (oesophageal mucosa). The patient is now asymptomatic and has seen been discharged from follow-up.
DISCUSSION
Our case presented with leiomyoma emanating from the upper oesophagus, which is rare as they are most frequently found in the mid to lower oesophagus correlating with the predominant muscular composition found in each of the regions; smooth muscle in the lower third and mixed (smooth/skeletal) muscle in the middle third. They usually appear intramurally our case presented intraluminally as a pedunculated mass with sudden onset symptoms of nausea and vomiting as opposed to the usual non-specific, longer duration symptoms of dysphagia, pain and weight loss (3).
Macroscopically leiomyomas are characterised as well circumscribed, smooth or nodular masses with a whorled cut surface (figure 2) and microscopically with bundles of smooth muscle cells intermingled with collagenous stroma (4).

Imaging modalities may include CT scanning to assess extra-oesophageal extent, barium swallow (filling defect) and endoscopic ultrasonography to assess which oesophageal layer the mass is in and its size, extent and nature (sold or cystic). Management options are non-operative (asymptomatic) or operative from enucleation via endoscopic, open or thorascopic methods to oesophageal resection and reconstruction for select tumours (greater than 8cm or adherent to the mucosa etc.) (3).
Anecdotally, a similar case was described by Simpson, 1934 of a lady coughing up a mass, which was subsequently swallowed. The patient was erroneously diagnosed as having globus hystericus and presented ten months later with a similar picture associated with sudden onset dysphagia. Furthermore, direct laryngoscopy confirmed a mass suspended by a pedicle from the area of the right piriform fossa hanging into the oesophageal entrance. This appeared to have twisted causing a haemorrhagic necrosis and the acute symptoms (5).
Our case describes the rare occurrence of an upper oesophageal leiomyoma presenting acutely as a large mass in the oral cavity. This diagnosis should be entertained as a differential in the circumstance of an odd-sounding referral of a patient who is reported to have ‘coughed up their tonsil’.



