-
PDF
- Split View
-
Views
-
Cite
Cite
Eu-Wing Toh, Ben Griffiths, Muhammad Farooq, An atypical presentation of colorectal cancer, Journal of Surgical Case Reports, Volume 2012, Issue 1, January 2012, Page 2, https://doi.org/10.1093/jscr/2012.1.2
Close - Share Icon Share
Abstract
Colorectal cancer is a common type of cancer in developed countries and is an important public health problem. Patients with colorectal cancer presents in a variety of ways in different settings. Most commonly, they present in the outpatient settings with changes in bowel habits, rectal bleeding and iron deficiency anaemia. This case reports an atypical presentation of colorectal cancer and how the cancer was diagnosed and treated.
INTRODUCTION
Colorectal cancer is the third most common cancer in the UK and approximately 37500 new cases are diagnosed each year (1). Patients with colorectal cancer commonly present to the outpatient setting with changes in bowel habit, rectal bleeding or iron deficiency anaemia. Cases are also identified via the national bowel cancer screening programme and another group of patients present acutely with bowel obstruction or perforation.
Outside these common modes of presentations, there are rare manifestations and we present such a case which demonstrates the value of modern imaging modalities and careful analysis of results.
CASE REPORT
A 78-year-old woman was admitted to our hospital with a week-long history of lethargy and lower back pain. She was found to be tender over her lumbar paraspinal muscles and was pyrexial. Laboratory investigations revealed iron deficiency anaemia (Hb – 9.8, Ferritin 8.0) and a raised C-reactive protein (324). An MRI scan of her spine shower L1/L2 discitis (figure 1) and she was commenced on intravenous antibiotics.

Sagittal view of MRI scans of spine confirming discitis of L1/L2 (indicated by arrow).
Urine microscopy was normal but blood cultures taken on the day of admission grew Escherichia coli (E. coli) and this, coupled with iron deficiency anaemia prompted a search for other pathology and a CT scan of chest, abdomen and pelvis showed thickening of the ascending colon (figures 2 and 3). A colonoscopy confirmed a fungating lesion in the mid-ascending colon and biopsies showed adenocarcinoma of the colon. Our patient then had a laparoscopic right hemicolectomy followed by adjuvant chemotherapy for a moderately differentiated adenocarcinoma (pT4 N2 V1 R0 M0). Her discitis settled with antibiotic treatment.
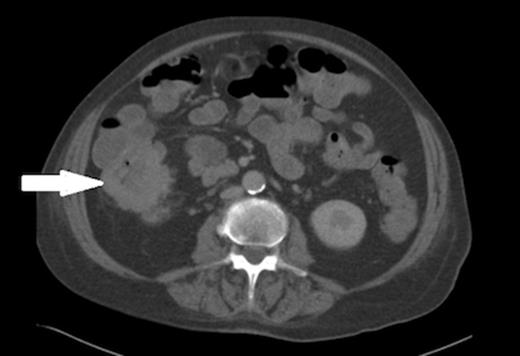
Axial view of the CT abdomen showing thickening of the ascending colon (indicated by arrow).
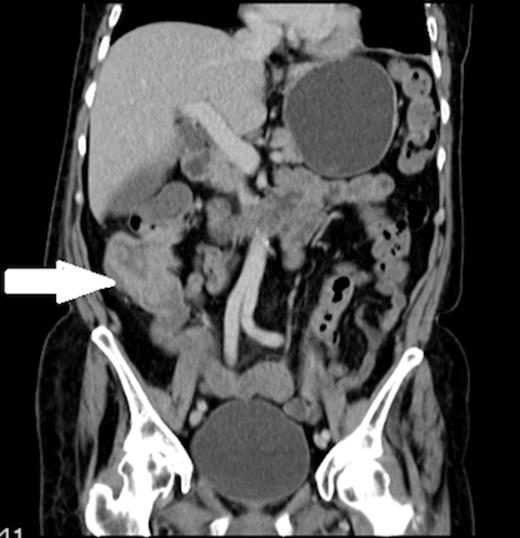
Coronal view of the CT abdomen showing thickening of the ascending colon (indicated by arrow).
DISCUSSION
Bacterial translocation is defined as the phenomenon by which organisms or their products escape from the intestinal tract to extra-luminal sites such as mesenteric lymph nodes, liver, spleen and the bloodstream (2). There are several factors that influence bacterial translocation including permeability of the gut mucosal barrier, host defence mechanism, immune status and type and load of gastrointestinal flora. These factors play a key role in determining the ease of bacterial translocation. It is known that bowel obstruction promotes bacterial translocation (3), but the pathophysiological significance of this process remains controversial in colorectal cancer. Some authors have suggested that although translocation takes place in bowel cancer patients, this is not of any clinical significance (4). It is thought that bacterial translocation occurs by intracellular passage but in colorectal cancer patients, the intestinal epithelium can also be penetrated by the extracellular route (5). The translocating bacteria can then spread to other sites in the body via the lymphatic and/or vascular route and cause infection at the distant sites. Bacterial endocarditis is well described in colorectal cancer (6,7) and septic arthritis has been also reported (8,9). We are aware of a case report of Streptococcus bovis discitis originating from colorectal malignancy (10) but we think this is the first reported case of E. coli discitis associated with colonic cancer.
With common diseases, it remains important to remember that atypical presentations do occur. It this case, the combination of iron deficiency anaemia and E. coli discitis alerted us to a possible gastrointestinal pathology and this was easily proven with cross-sectional imaging and subsequent colonoscopy.
This case lends support to the hypothesis of bacterial translocation during periods of intestinal disease and the locally advanced nature of the cancer would seem to have allowed route of bacterial passage via the lymphatic or vascular route.
REFERENCES
References Cancer Research UK. Cancer Stats: http://info.cancerresearhuk.org/cancerstats/types/bowel/ [Accessed 10th June 2011]



