-
PDF
- Split View
-
Views
-
Cite
Cite
H Bukhari, M Ayad, A Rosenthal, M Block, M Cortelli, Superior vena cava syndrome secondary to thyroid cancer, Journal of Surgical Case Reports, Volume 2011, Issue 7, July 2011, Page 7, https://doi.org/10.1093/jscr/2011.7.7
Close - Share Icon Share
Abstract
It is uncommon for thyroid cancer to present with superior vena cava syndrome. Obstruction of superior vena cava can develop as a result of intrinsic and extrinsic spread of the thyroid cancer. The usual presentation of this disease entity is a neck mass with symptoms and signs suggestive of superior vena cava obstruction. Superior vena cava obstruction is commonly caused by lung cancer and lymphoma. However, thyroid cancer can cause superior vena cava obstruction by downward tumour spread into the mediastinum causing extrinsic compression, which will lead to narrowing and thrombosis of the major venous system in the chest. Paraganglioma can also present with superior vena cava obstruction and it mimics thyroid cancer microscopically. Proper staining should be performed to differentiate between the two diseases. This could be the first case of this kind reported in the literature.
INTRODUCTION
Superior vena cava (SVC) obstruction secondary to thyroid cancer is extremely rare. This case describes a patient with thyroid cancer who suffered complete superior vena cava obstruction as a result of follicular carcinoma metastasis into the SVC, creating a massive venous thrombus. The tumour was thought preoperatively to be a paraganglioma, but the correct diagnosis was made intraoperatively by frozen section. The patient underwent resection of the tumour and SVC, with concomitant total thyroidectomy and subsequent postoperative radio-iodine ablation therapy.
CASE REPORT
A 67-year old gentleman presented with progressive head and neck swelling and discomfort for several months. His symptoms were pronounced by bending over or straining in the bathroom. His symptoms worsened and he was referred for thoracic surgery consultation after a mass was seen on chest x-ray. He was diagnosed with SVC syndrome secondary to a mediastinal mass, demonstrated best by computed tomography (CT) [Figures 1, 2, 3].
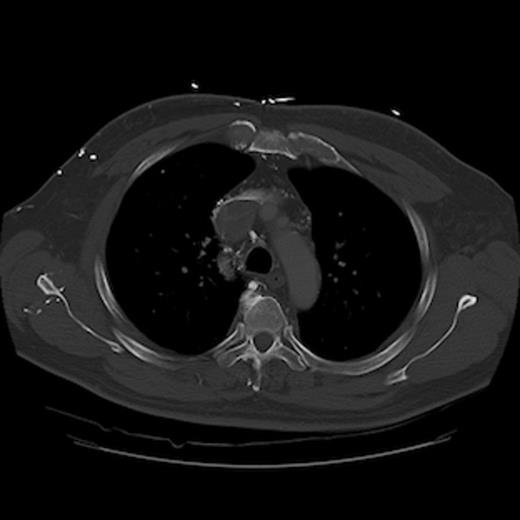
CT of the chest (axial section) with intravenous contrast: demonstrates complete obstruction of the superior vena cava with a large intramural thrombus
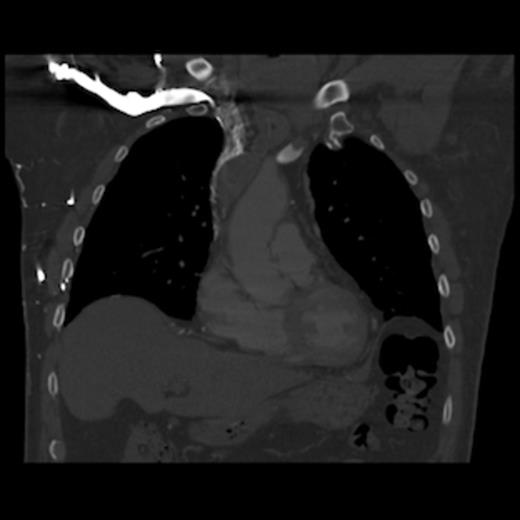
CT of the chest (coronal section) with intravenous contrast: demonstrates complete obstruction of the superior vena cava by a large intramural thrombus that extends into brachiocephalic vein
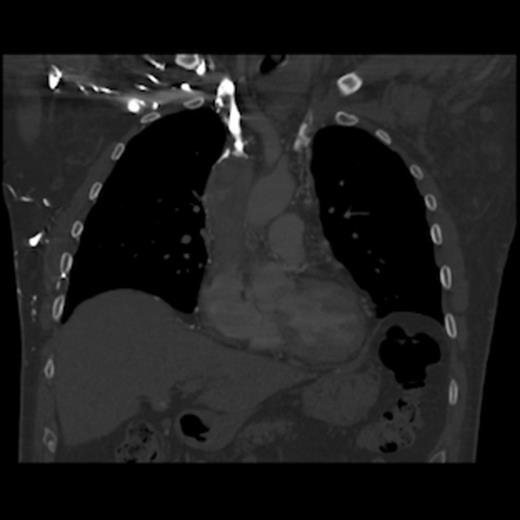
CT of the chest (coronal section) with intravenous contrast: demonstrates large thrombus obstructing the superior vena cava down to the right atrium
The thyroid gland was noted to be homogeneously enlarged and (a random?) fine needle aspiration was performed by ultrasound guidance. CT-guided biopsy of the mediastinal mass showed nests of epithelioid cells with clear cytoplasm and organoid pattern. The tumour stained positive for vimentin. Staining for thyroglobulin was not performed. Biopsy of the mediastinal mass was labeled paraganglioma [figure 4] and of the thyroid, a benign goiter. Thyroid function testing was normal.
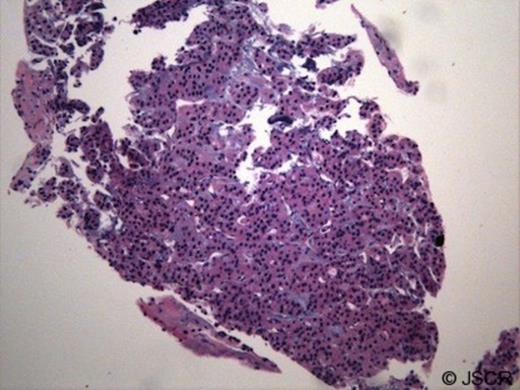
Microscopic examination of the mediastinal mass biopsy (H and E stain): revealed tumour cells with benign appearance and histologic features consistent with paraganglioma
The patient was taken to the operating room for tumour resection with reconstruction of the superior vena cava. The mass extended from the mediastinum into the inferior thyroid veins, with frozen section margins demonstrating thyroid cells. Metastatic thyroid cancer was diagnosed. Total thyroidectomy was performed through a distinct transverse cervical incision. The gland was enlarged and moderately fibrotic. There was no discrete mass and no gross lymphadenopathy. The inferior thyroid veins were engorged and felt like enlarged lymph nodes.
Following surgery, the patient recovered uneventfully and was discharged. Final pathology of the thyroid gland showed follicular carcinoma with Hurthle cell features [Figure 5].
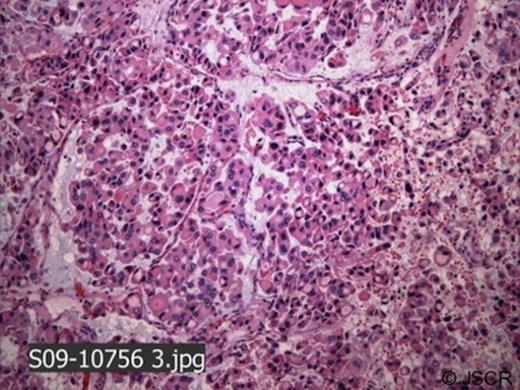
Microscopic examination of resected thyroid gland (H and E stain) demonstrates invasive thyroid follicular carcinoma with hurthle cell features and extensive angioinvasion.
There was both capsular and extensive angioinvasion. The thyroid tumour was found within the lumen of SVC causing complete occlusion. The patient has since undergone radioactive iodine ablation therapy.
DISCUSSION
Neoplastic SVC occlusion is usually secondary to lung cancer or lymphoma, but can also be due to advanced thyroid tumours (1,2,3). This case of SVC syndrome was due to an aggressive thyroid follicular carcinoma with extensive angioinvasion and venous spread. Our patient had a typical presentation of SVC syndrome with neck and head swelling and fullness, but the cause of his obstruction was initially believed to be a large paraganglioma, based on the pathology from his CT-guided biopsy. Paraganglioma can mimic thyroid cancer histologically, and special staining is required to differentiate the two diseases. Ideally, immunohistochemistry should be performed but this is not always available (4,5). Frozen section is extremely useful because in this situation, the presence of follicular thyroid cells outside the gland is diagnostic of thyroid carcinoma. A second surgery to perform thyroidectomy is thus avoided by the accurate frozen section histology.
Hurtle cell carcinoma is a variant of follicular thyroid carcinoma. Metastasis is almost always haematogenous. Aggressive surgical resection is the best current treatment because the tumour is usually less responsive to radioactive iodine ablation than the more common generic follicular carcinoma. Most tumours are treated with total thyroidectomy followed by I131 therapy. Subsequent lifelong thyroid suppression therapy is the norm, and recurrence is usually best treated with resection.
The surgeon should examine the thyroid of all patients with SVC syndrome and consider thyroid cancer as a possible cause when a thyroid nodule is present, particularly when the patient is a nonsmoker. All patients with SVC syndrome and thyroid nodules should undergo biopsy of the thyroid to aid in planning the extent of surgical resection and postoperative therapy.
Thyroid cancer can cause intraluminal SVC obstruction from venous metastases. This can occur in the absence of an obvious mass in the thyroid gland or in the mediastinum. Patients with SVC syndrome should have a careful thyroid exam and the diagnosis should be considered when there is a solid thyroid nodule present. When SVC syndrome is secondary to metastatic thyroid cancer, aggressive surgical resection should include the thoracic and cervical disease and total thyroidectomy should be performed.



