-
PDF
- Split View
-
Views
-
Cite
Cite
S Lal, Y Kailasia, S Chouhan, APS Gaharwar, GP Shrivastava, Delayed presentation of post traumatic diaphragmatic hernia, Journal of Surgical Case Reports, Volume 2011, Issue 7, July 2011, Page 6, https://doi.org/10.1093/jscr/2011.7.6
Close - Share Icon Share
Abstract
Blunt traumatic diaphragmatic rupture is an uncommon but severe problem that is usually seen in polytraumatized patients including blunt abdomino-thoracic trauma due to road traffic accidents, fall from height and penetrating injuries. Regardless of the mechanism, diagnosis is often missed and high index of suspicion is vital. Late presentations are associated with increased morbidity. We report an interesting case of blunt traumatic diaphragmatic hernia in a 32-year-old man presenting 4 years after the initial abdomino-thoracic injury due to fall from height. He had herniation of the spleen and stomach. Through a left sub costal incision, the herniated organs were reduced and diaphragmatic defect closed with interrupted prolene suture.
INTRODUCTION
Blunt traumatic rupture of the diaphragm is a serious injury that is often difficult to diagnose. (1) It is an uncommon injury whose incidence is rising because of the increasing number of road traffic accidents in the last few years, together with better pre-hospital and hospital resuscitation of severely injured patients and improved diagnostic facilities. (2) In developing countries where initial care of severely injured patients and diagnostic facilities are less than optimal, blunt traumatic diaphragmatic rupture (BTDR) may go undiagnosed. High index of clinical suspicion is required because of the missed diagnosis and potential for delayed presentation. We report a case of delayed presentation of post traumatic diaphragmatic hernia and reviewed the literature to highlight challenges in diagnosis and management of such cases.
CASE REPORT
A 32 year old male was admitted to the emergency department with a history of nausea, vomiting, pain in the chest and upper abdomen as well as breathlessness of 3 days duration. He had a history of blunt trauma to the abdomen following a fall from a tree 4 years previously. He was then treated conservatively and no diaphragmatic hernia was detected. On physical examination the patient appeared pale, dehydrated and had dyspnea. Examination of the left chest showed decreased movement on respiration, absent breath sounds, bowel sounds were present and dullness on percussion. Apart from a mild anaemia (9gm/dl), all blood tests were within normal limits. The chest X-ray showed a large air-fluid level in the left thoracic cavity with a nasogastric tube within it, collapse of left lung field, obliteration of cardio-phrenic angle and shifting of the mediastinum toward the right side. (Figure 1)
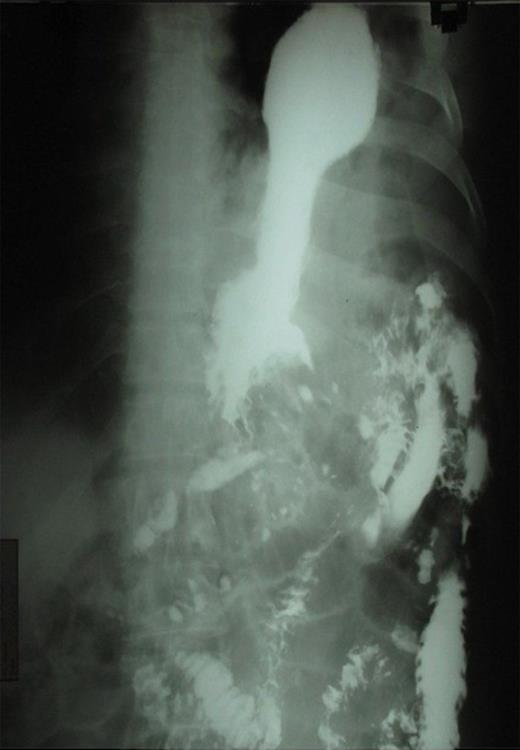
The presence of the nasogastric tube was confirmed with the presence of gurgling sound on auscultation after administration of air through it. Barium meal was carried out to localize the stomach and showed the presence of the stomach in the thoracic cavity confirming diagnosis of post-traumatic diaphragmatic hernia. (Figure 2)
The patient was counseled and prepared for surgery through a left sub costal incision. The findings at surgery were that two-thirds of the stomach, omentum and spleen had herniated through a 10cm X 7cm tear in left hemidiaphragm into the chest. (Figure 3) Contents were normal and reduced into the abdomen. An intercostal chest tube drain was guided in the left thoracic cavity. Diaphragmatic tear was repaired with horizontal mattress prolene suture. Postoperative period was uneventful. Follow-up after 1 year showed no recurrence.
DISCUSSION
Diaphragmatic injuries were described first by Sennertus in 1541. Riolfi performed the first successful repair in 1886. Not until 1951, when Carter et al., published the first case series, was this injury well understood and delineated. (3) Approximately 0.8%-1.6% of patients with blunt trauma shows a rupture in the diaphragm. (4) Blunt trauma accounts for 75% of ruptures, and penetrating trauma accounts for the rest. Approximately 69% of hernias are left-sided, 24% are right-sided, and 15% are bilateral. (5,6)
Patients with delayed diaphragmatic herniation frequently present months to years after the initial injury with manifestations of visceral herniation, incarceration, obstruction, ischemia from strangulation, or perforation. In our case, symptoms of diaphragmatic hernia developed 4 years later. Symbas et al., observed a delay in diagnosis in 8% of cases of diaphragmatic injury from 18 h to 15 years after injury. (7) Chest radiography is the standard in the advanced trauma life support (ATLS) protocol for a trauma workup. Approximately 23-73% of traumatic diaphragmatic ruptures will be detected by initial chest radiograph, with an additional 25% found with subsequent films. Chest radiographic findings that indicate traumatic rupture include the following (8):
Abdominal contents in the thorax, with or without signs of focal constriction (“collar sign”)
Nasogastric tube seen in the thorax,
Elevated hemidiaphragm (>4 cm higher on left vs right) and
Distortion of diaphragmatic margin.
Barium meal usually confirms presence of cardia and fundus of stomach above the diaphragm. When BTDR occurs without herniation, diagnosis becomes even more difficult. Conventional CT scan has been reported to have a sensitivity of 14%-82%, with a specificity of 87%. Helical CT has increased sensitivity 71-100%, with higher sensitivity for left vs right. CT findings indicating rupture include the following (8):
Direct visualization of injury
Segmental diaphragm non-visualization
Intrathoracic herniation of viscera
“Collar sign’’
Peridiaphragmatic active contrast extravasation
Ultrasonography (focused assessment with sonography for trauma [FAST] scan) has been reported to detect diaphragmatic hernias. (9) Our patient was diagnosed by abdomino-thoracic x-ray and barium meal study.
Surgery is the mainstay in the treatment of diaphragmatic rupture. (10) Operative repair is technically more difficult if the surgery is delayed. The difference is based on the degree of adhesion present in the thoracic cavity and the state of the herniated organs. After reduction of the abdominal contents, the diaphragm is usually repaired simply with monofilament nonabsorbable suture as in our case.
Delay in presentation of a diaphragmatic hernia in this case could be explained by various hypotheses. Delayed rupture of a devitalized diaphragmatic muscle may occur several days after the initial injury. However the more likely explanation is a possible delayed detection assuming that the diaphragmatic defect occurring with injury manifests only when herniation occurs.
In conclusion, a history of trauma must be investigated to diagnose patients with a delayed post traumatic diaphragmatic hernia. A high index of suspicion and the use of relevant radiological investigation is essential for early diagnosis. All cases whether diagnosed pre-operatively or intraoperatively must be repaired surgically either by laparotomy, thoracotomy, a thoraco-abdominal approach or by minimal access surgery. Laparotomy should be the preferred approach in unstable patients.





