-
PDF
- Split View
-
Views
-
Cite
Cite
M Jayant, R Kaushik, Cocoon within an abdominal cocoon, Journal of Surgical Case Reports, Volume 2011, Issue 5, May 2011, Page 7, https://doi.org/10.1093/jscr/2011.5.7
Close - Share Icon Share
Abstract
Intestinal obstruction is a fairly common surgical emergency that usually occurs due to herniae, adhesions, or bands. Rarely, uncommon causes such as an abdominal cocoon are encountered, where part or all of the small intestine is encased within a thin membrane. We report one such case of abdominal cocoon, in whom, further encasement of the distal ileum was seen within a separate membrane.
INTRODUCTION
The abdominal cocoon is an infrequently encountered cause of intestinal obstruction that was was first observed by Owtschinnikow in 1907, and later, termed the ‘cocoon’ by Foo in 1978. The exact aetiology of this entity (also called ‘scerosing encapsulating peritonitis’) is by and large unknown (the idiopathic/primary variety of cocoon), but at times, cocoon formation can occur secondary to a variety of conditions (secondary cocoon) like drugs (practolol, propranolol), chronic ambulatory peritoneal dialysis, ventriculoperitoneal shunts, diseases such as sarcoidosis, SLE, liver cirrhosis, uterine leiomyomas, endometriotic cysts or tumours of the ovary, etc. Tuberculosis has also been reported as a cause of abdominal cocoon, altbeit rarely. (1,–,4)
We report the unusual case of a young female patient with repeated episodes of intestinal obstruction due to further encasement of the distal ileum within a separate membrane that was wholly within the outer covering cocoon – a ‘cocoon within a cocoon’.
CASE REPORT
A 16 year old female patient presented to us repeatedly with episodes of small bowel obstruction that had previously responded to conservative management. This time, she had a vague mass in the right iliac fossa in addition to her obstructive features. Although she responded to conservative management this time also, the mass did not disappear.
A computerised tomogram (CT) scan was done to assess the mass, which revealed a fixed obstruction at the terminal ileum along with dilatation of the small bowel above. A laparotomy was performed after adequate preparation. At laparotomy, the whole of the stomach, small bowel and part of the ascending colon were encased by a thin membrane (Figure 1).
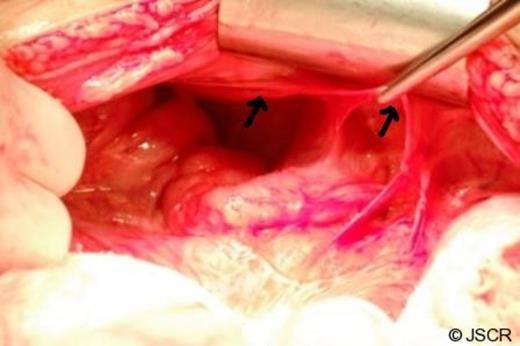
Thin membrane that was encasing the stomach, small intestine and part of the ascending colon (black arrows)
Once this membrane was opened up, it was found that the terminal ileum was jumbled up and encased within another thick membrane (Figure 2) that was separate from the outer covering. This was lysed, and the small bowel within it freed. There was no other obvious pathology at surgery. A biopsy of both the membranes was sent for analysis.
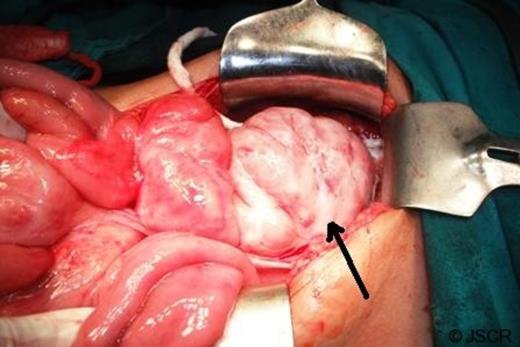
Jumbled up terminal ileum encased within another thick membrane (black arrow)
The post operative period was uneventful. The histopathology report of the two membranes was non-specific, and did not reveal any evidence of tuberculosis. The patient is well on a follow up of nearly 6 months.
DISCUSSION
Since it was first reported in 1907, the abdominal cocoon still remains uncommon as a cause of intestinal obstruction. A search on Pubmed revealed only about 92 articles on this topic (abdominal cocoon) to date. As mentioned earlier, the cocoon can arise as a primary disease when there is no obvious etiology, or it can be secondary, in the setting of various factors as have been listed. The primary form of the disease is much more common than the secondary form, and is seen usually in young females, especially from the tropical or subtropical countries. Although the etiology is not known, it has been hypothesised that it may arise as a response to subclinical primary viral peritonitis, gynecological infections, or retrograde menstruation (3). However, as the primary abdominal cocoon has been seen to occur in all ages, and even in males, casts some doubt on these factors solely being involved in the pathogenesis of the primary form of this unusual disease. The offending condition is more obvious in the secondary form of abdominal cocoon, where bowel encapsulation occurs in the presence of a variety of factors listed previously.
It is uncommon for the diagnosis to be made with confidence preoperatively, since these patients present with non-specific signs and symptoms such as colicky abdominal pain, emesis and recurrent episodes of intestinal obstruction. There are no specific radiological features of the disease that can give the diagnosis with certainty. Plain x-rays of the abdomen may reveal evidence of small bowel obstruction – dilated bowel loops and air-fluid levels. Abdominal ultrasound or small bowel barium studies may show a ‘cauliflower’ appearance in which the intestinal loops are arranged in a concertina shape with a narrow base. A CT scan may show dilated ileal loops towards the centre of the abdomen, or even, encasement by a membrane (5).
However, it is often only at laparotomy (5) or during laparoscopy that the actual diagnosis is made, when part or whole of the small bowel is seen encased within a sac. Although the sac usually encases the small bowel, at times, it can extend to involve the colon, liver and even the stomach. Lysis of this sac is sufficient to relieve obstruction in most cases, but in a tubercular cocoon, it has been our experience that there are further adhesions between bowel loops that require adhesiolysis (3). However, in the absence of obvious evidence of tuberculosis within the abdomen, the diagnosis of tuberculosis as a cause of cocoon is only made with certainty following histological analysis.
The presentation reported here is unusual in that there was encasement of the terminal ileum within a sac, and this itself, along with rest of the small bowel, stomach and ascending colon was encased within a larger sac. Despite an extensive search of available literature, we could not come across any similar case in which bowel being encased within a cocoon, that itself was encased within a larger cocoon, as reported here – an abdominal cocoon within a cocoon!



