-
PDF
- Split View
-
Views
-
Cite
Cite
A Peter, M Walker, K Shinil, D Shah, A Eduardo, M Souchon, G Stefanos, M Millas, Biliary stent migration presenting as transdiverticular sigmoid perforation, Journal of Surgical Case Reports, Volume 2011, Issue 3, March 2011, Page 6, https://doi.org/10.1093/jscr/2011.3.6
Close - Share Icon Share
Abstract
The authors present a case report of a patient with distal plastic biliary stent migration resulting in perforation through a sigmoid diverticulum. The perforation was contained by a loop of ileum that had descended into the pelvis allowing for a sigmoid resection with primary anastomosis. This rare complication of biliary stent placement should be included in differential diagnosis of any patient that presents with lower quadrant abdominal pain after endoscopic retrograde cholangiopancreatography with stent placement.
CASE REPORT
The patient being reported is a 69 year old female with a history of cholecystitis, coronary artery disease requiring percutaneous stent placement, dyslipidemia, hypertension, hypothyroidism, and depression. She had a remote history of open cholecystectomy for cholecystitis many years prior to presentation. She initially presented to our institution in May 2010 complaining of several days of nausea, emesis, feeding intolerance, and diffuse abdominal pain. Laboratory parameters were remarkable for a mild elevation in her hepatic transaminases (alanine aminotransferase (ALT) of 106, and aspartate aminotransferase (AST) of 111) as well as an alkaline phosphotase of 144. Diagnostic imaging included a computed topography (CT) scan of the abdomen and pelvis as well as abdominal ultrasound that showed a dilated common bile duct to 1.1 cm and sigmoid diverticulosis. The patient subsequently underwent endoscopic retrograde cholangiopancreatography (ERCP) showing a distal common bile duct stricture. A sphincterotomy was completed followed by placement of a 7 cm 10 French plastic biliary stent. Brushings complete of the site of stricture were negative for malignancy. The patient did well clinically after the procedure and was discharged home.
The patient returned to clinic for a repeat outpatient ERCP approximately 3 months after her initial presentation for re examination and stent removal. Findings included absence of the biliary stent with continued dilation of the common hepatic and common bile ducts to 1.1 cm. A repeat sphincterotomy was performed with completion cholangiogram showing no obstruction in the biliary tree. As the patient was asymptomatic from the stent migration she was discharged home without further incident.
Five months after initial presentation, the patient presented to the emergency department complaining of a 3 day history of fever, nausea, emesis, feeding intolerance, diarrhoea, and left lower quadrant abdominal pain. She was found to be febrile to 101.7oF and tachycardic to 108. Laboratory parameters were significant for a leukocytosis of 12,000 (per µL) associated with 90% neutrophils and 6% bands. A CT scan of the abdomen and pelvis showed a foreign body in the sigmoid colon lumen that had perforated through the bowel wall. An adjacent 2.1 cm fluid collection was identified with surrounding fat stranding and small bowel wall thickening (Figure 1). The patient was resuscitated, started on broad spectrum antibiotics, and taken urgently to the operating room for exploratory laparotomy.
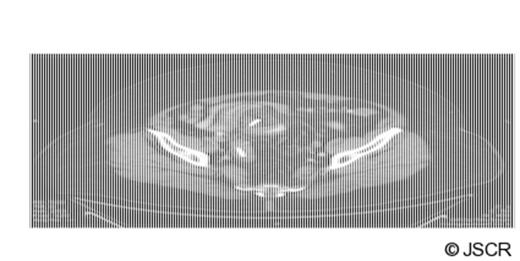
Cross sectional and coronal images of biliary stent in the sigmoid colon lumen with perforation through the bowel wall and surrounding abscess cavity
Intra-operative findings included dense intra abdominal adhesions and multiple sigmoid diverticula. The biliary stent had migrated into the distal sigmoid colon just proximal to the rectosigmoid junction. Additionally, the stent had lodged itself into and perforated through a sigmoid diverticulum. Fortunately, the perforation was contained by a loop of distal ileum and adjacent omentum that had descended in the pelvis (Figure 2). The sigmoid colon was resected and an end to end stapled anastomosis was fashioned. The patient had an uncomplicated post operative course and was discharged home. Final pathology showed colonic diverticula with fistula track and surrounding acute inflammation.
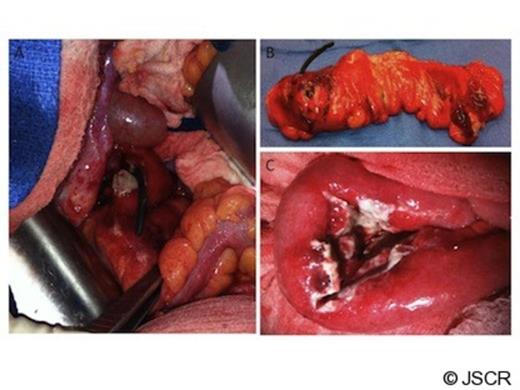
(A) Perforation of plastic biliary stent through sigmoid colon wall in vivo. (B) Perforation of plastic biliary stent through sigmoid colon wall ex vivo. (C) Abscess cavity shown to be contained within a loop of small bowel.
DISCUSSION
Current medical practice often employs plastic biliary stents for the treatment of benign obstructive biliary disease. A recent review of 204 plastic biliary stent placement procedures for benign disease showed a migration rate of 13.4% with an equal proportion of stents found in the proximal and distal gastrointestinal tract. All of the migrated stents were retrieved without complication (1).
Few cases of complicated stent migration causing colonic perforation requiring operative intervention have been reported in the literature (2,3,4,5). These rare cases describe delayed presentation with localized abdominal pain after metal or plastic biliary stent placement. All patients were treated with colonic resection followed by primary anastomsis or Hartman’s procedure.
Our case is unique as the stent was found to be lodged within a sigmoid diverticula and it appeared that chronic inflammation caused perforation. The perforation was contained by a loop of distal small bowel that had descended into the pelvis (as show in Figure 2). The containment of the fecal material kept the patient from developing diffuse peritonitis and sepsis. Additionally, the contained perforation ensured un-inflamed proximal and distal margins after sigmoid colectomy allowing for primary anastomosis.
Biliary stent migration complicated by sigmoid colon perforation is a rare event that should be included on the differential during work up for abdominal pain after ERCP with stent placement. Additionally, if the perforation is contained with healthy un-inflamed margins after sigmoid colectomy, a primary anastomosis is a reasonable treatment option.



