-
PDF
- Split View
-
Views
-
Cite
Cite
J Glaser, J Pearl, G Wind, F Sheppard, Laparoscopic repair of a large interstitially incarcerated inguinal hernia, Journal of Surgical Case Reports, Volume 2011, Issue 3, March 2011, Page 2, https://doi.org/10.1093/jscr/2011.3.2
Close - Share Icon Share
Abstract
A 68 year old female presented for elective repair of an abdominal wall hernia. Preoperative CT imaging revealed a right inguinal hernia defect with hernia contents coursing cephalad between the external and internal abdominal oblique muscles. This was consistent with an interstitial inguinal hernia, a rare entity outside of post- traumatic hernias. At operation the hernia contents were reduced laparoscopically. The hernia was then repaired by transitioning to the totally extraperitoneal (TEP) approach using a 15cm X 15cm piece of polyester mesh. The patient had an uneventful recovery. Interstitial hernias are rare, difficult to diagnose and potentially dangerous if left untreated. There is no consensus on the ideal repair of these unique hernias. This represents a minimally invasive repair of an unusual hernia, with a novel approach to diagnose and manage the hernia and its redundant sac.
INTRODUCTION
The hernia sac of indirect inguinal hernias usually remains within the inguinal canal or courses caudad into the scrotum or labia. In anterior abdominal wall interstitial hernias, the sac insinuates between either the external oblique and internal oblique muscles or the internal oblique and transversus abdominus muscles. Interstitial hernias are rare entities and are generally encountered in the setting of previous abdominal wall trauma or exist in the settings of congenital defects such as aberrant descent of the testes. We present a rare case of a non-traumatic interstitial hernia repaired with a combined transabdominal and extraperitoneal laparoscopic approach.
CASE REPORT
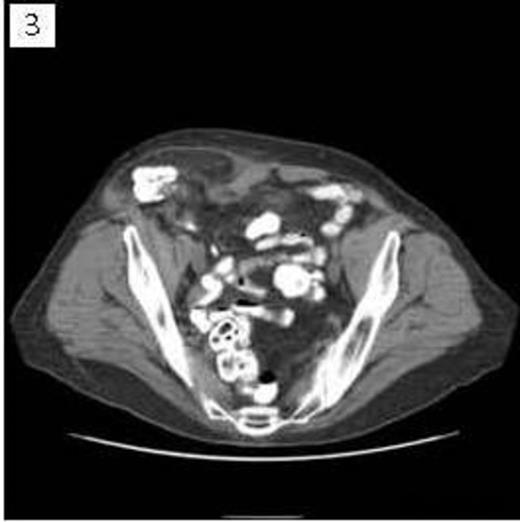
A 68 year old female presented to clinic with a several year history of right lower quadrant abdominal discomfort and “bulge”. Physical exam demonstrated a reducible mass originating in the inguinal region that tracked cephalad above the level of the inguinal ligament. CT imaging revealed a large inguinal hernia defect (Figure 1) with herniated bowel coursing 13cm cephalad between the external and internal abdominal oblique muscles (Figure 2 & 3).


Diagnostic trans-abdominal laparoscopy was performed to evaluate the intestines, define the hernia defect anatomy, and attempt hernia reduction. Exploration revealed normal appearing bowel and a large right sided indirect hernia defect and the hernia contents were reduced without undue difficulty (Figure 4).
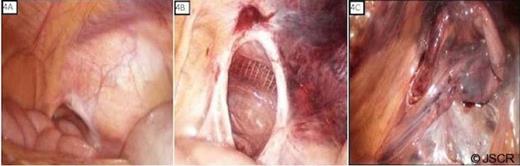
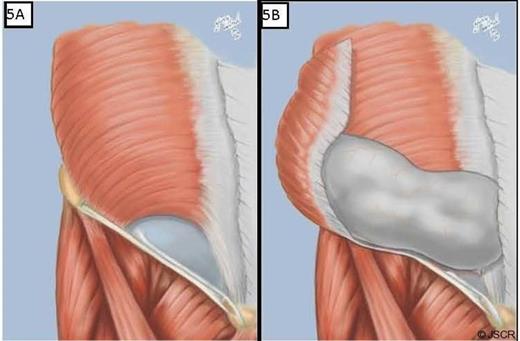
The trans-abdominal laparoscopic ports were left in position and additional laparoscopic ports place for a totally extraperitoneal approach for repair. After adequate dissection of the preperitoneal space and reduction of the hernia sac, a 15cm X 15cm polyester mesh was used to broadly cover the direct, indirect and femoral spaces. The laparoscope was then reinserted transabdominally to ensure wide mesh overlap of the defect (Figure 5).
There was a large redundant hernia sac with a wide opening, worrisome for potential internal herniation of abdominal contents; the hernia sac was folded over itself and tacked to the abdominal wall, above the level of the anterior superior iliac spine, to prevent this risk. The patient had an uneventful post-operative recovery and there is no evidence of recurrence 12 months post-repair.
DISCUSSION
Interstitial hernias were first described in 1661 by the Danish physician Thomas Bartholin(1), but it was not until 1797 that Jean Petit first defined this hernia anatomically. The term interstitial hernia, occasionally used interchangeably with interparietal hernia, refers to a hernia sac found between the various layers of the abdominal wall and is further classified according to the layer it is found between(2). It has been described as congenital (3), associated with abnormal descent of the testis (4), or associated with recurrence following a mesh hernia repair (5).
Though interstitial hernias are rare (0.07% of all hernias), they have a predilection for incarceration and strangulation. Diagnosis by physical exam alone can be very challenging; potentially leading to a delay in diagnosis and poor patient outcome. It is reported that the longer an interstitial hernia goes without operative repair the more unfavorable the operative outcome will be (2). With the use of modern imaging the accuracy of diagnosis is improved, however these remain clinically rare and potentially dangerous hernias.
There is little in the literature regarding the optimal approach to and repair of interstitial hernias. The original descriptions of its repair are with an open, anterior technique, initially with tissue repairs and then later with mesh. Other reports indicate that a laparoscopic repair is adequate. We chose to repair this hernia in the preperitoneal space with mesh with the addition of trans-abdominal laparoscopy for wide visualization and inspection of the bowel and redundant hernia sac involution.
The initial trans-abdominal approach allowed for confirmation that this hernia was inguinal in origin, reduction and inspection of the bowel. We followed this with a traditional TEP repair, with balloon dissection of the preperitoneal space, clearance of the direct, indirect, femoral and obturator spaces and placement of a large polyester mesh. At completion of the repair, trans-abdominal inspection revealed a redundant hernia sac with a large, fibrous neck, opening, worrisome for subsequent internal herniation. Additionally, there was a small peritoneal defect that exposed the preperitoneal mesh to the abdominal cavity, by involution and pexy of the hernia sac to the abdominal wall the redundant sac and risk of internal herniation and complete coverage of mesh was accomplished. As a consequence of a minimally invasive approach, the patient was discharged the day following surgery and at 12 months post-operatively there is no evidence of recurrence and the patient is symptom free.
Interstitial hernias are rare, difficult to diagnose and potentially dangerous if left untreated. There is no consensus on the ideal repair of these unique hernias. While laparoscopic repair of interstitial hernias is not novel, its use in large, incarcerated hernias can be challenging. Utilizing a combination of trans-abdominal and extraperitoneal laparoscopy was efficient and efficacious in the case presented. This represents a novel minimally invasive approach to an unusual hernia that permitted safe, efficient and efficacious evaluation and management of an incarcerated interstitial hernia and risk reduction of a potential internal herniation.



