-
PDF
- Split View
-
Views
-
Cite
Cite
P Vulliamy, A Srilekha, N Fotiadis, C Kyriakides, Operative repair of an incidentally diagnosed giant hepatic artery aneurysm, Journal of Surgical Case Reports, Volume 2011, Issue 3, March 2011, Page 1, https://doi.org/10.1093/jscr/2011.3.1
Close - Share Icon Share
Abstract
Hepatic Artery Aneurysms (HAA) are rare vascular lesions which are associated with significant morbidity and mortality in the event of rupture. Early diagnosis and expedient management are therefore important to optimise outcome. Here we report a case of a giant Hepatic Artery Aneurysms (HAA) found incidentally on Computerised Tomography, successfully managed without complication by elective surgical repair.
INTRODUCTION
Hepatic Artery Aneurysms (HAA) are rare but clinically significant entities, owing to the high rates of spontaneous rupture and subsequent high mortality. Asymptomatic in up to a third of cases, HAA are increasingly diagnosed incidentally during radiological investigations for other pathology.(2)Early diagnosis and repair before rupture occurs is clearly preferable, and morbidity and mortality of elective surgical or radiological intervention appears to be low.(3)Here we present an incidental finding of an asymptomatic giant HAA and successful elective surgical repair.
CASE REPORT
A 74 year-old female with a background of diverticular disease, hypertension, and type 2 diabetes mellitus was admitted with a three-day history of rectal bleeding. On admission the patient was haemodynamically stable with a pulsatile, non-tender mass palpable in the epigastrium and tenderness in the left iliac fossa. No bruit was heard on auscultation. She underwent a CT scan, which revealed an incidental finding of a large saccular aneurysm involving the common hepatic artery and the hepatic artery proper, measuring 6.2 x 7.1 x 7.5cm in maximum dimensions (Figure 1). In addition, multiple focal dilatations of medium-sized visceral arteries (including the splenic artery and left renal artery) were identified.
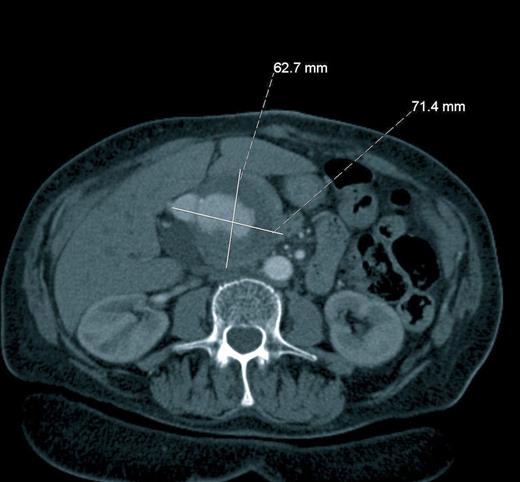
Axial Computerised Tomography scan after administration of intravenous contrast showing a giant hepatic artery aneurysm
Owing to the proximity of the aneurysm neck to the bifurcation of the hepatic artery and lack of landing zone for the stent, the aneurysm was not felt to be suitable for endovascular repair. Open surgery was therefore performed, with exposure of the aneurysm through a midline incision (Figure 2) and repair using an interpostion long saphenous vein inlay graft to exclude the aneurysm sac.
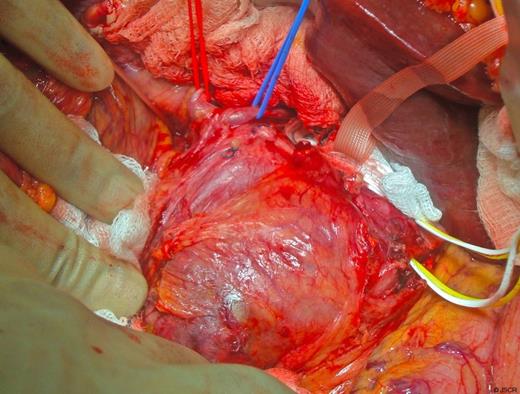
Intraoperative image showing the aneurysm arising from the common hepatic artery (white sling) and its relationship to the left and right hepatic arteries (red and blue slings)
Post-operatively the patient was transferred to the Intensive Care Unit for ongoing monitoring. She made a good recovery with no immediate or early complications, and was discharged home after one week. She remains asymptomatic 6 months post-operatively, with graft patency confirmed on duplex ultrasonography.
DISCUSSION
True hepatic artery aneurysms, particularly those of the dimensions described in this case, are rare vascular lesions. Frequently atherosclerotic in origin, they may also be due to vasculitides – such as Polyarteritis Nodosa – and inherited connective tissue disorders.(4) Clinical presentation ranges from incidental detection of asymptomatic aneurysms on ultrasound or Computerised Tomography, to acute abdominal pain and cardiovascular collapse in the event of rupture, which carries a mortality in the region of 40%.(1) HAA are thus an important, if rare, diagnosis to consider in the patient presenting with right upper quadrant pain and haemodynamic instability. Symptoms such as obstructive jaundice and gastrointestinal bleeding can also occur,(5) and may be mistakenly attributed to more common conditions.
There are few reports of management strategies for giant HAA in the literature, and as such the optimal treatment remains controversial. Several studies have demonstrated the efficacy and safety of endovascular management of visceral artery aneurysms including giant HAA.(6) Elective open surgical repair of HAAs has also been shown to be associated with high success rates and low complication rates in both the short and long-term.(7) As this case demonstrates, surgery may be the most appropriate option in cases where the anatomical characteristics of the aneurysm preclude against endovascular repair. In either case, expedient repair before rupture occurs is essential once the diagnosis has been made.



