-
PDF
- Split View
-
Views
-
Cite
Cite
Seif J Uledi, A rare gigantic solitary cysticercosis pseudotumour of the neck, Journal of Surgical Case Reports, Volume 2010, Issue 9, November 2010, Page 5, https://doi.org/10.1093/jscr/2010.9.5
Close - Share Icon Share
Abstract
Cysticercosis is one of the ancient parasitic infections and endemic in many parts of the developing world. Humans acquire cysticercosis when they ingest pork tapeworm eggs either through faecal-oral route by eating faecally contaminated food or by auto infection.
The clinical picture largely depends on the location of larval encystment. Neurocysticercosis is the most common form of presentation. Solitary extra neural lesions are quite rare and fairly small in size.
We present a very unique case of 56 year old Malawian female with a very rare, long standing gigantic solitary cysticercosis pseudo tumour of the neck. By far, there is no documented report on incorrigible cysticercosis lesion with such a sheer size.
Solitary extraneural cysticercosis lesions may mimic other soft tissue masses; therefore it is important for clinicians working in endemic regions to consider cysticercosis as a differential diagnosis when evaluating patients with soft tissue lesions.
INTRODUCTION
Cyticercosis is a systemic parasitic infestation caused by the pork tapeworm, Taenia solium. This tapeworm is endemic to many parts of the developing world including Latin America, Asia and Sub-Saharan Africa. However, due to population dynamics there has been an increase of cysticercosis cases reported from the non-endemic areas (1)
Two forms of cysticercosis manifestation are known, the neurocysticercosis and extra neural cysticercosis. In English literature a fair number of solitary extra neural cysticercosis lesions have been reported. However, to the author’s knowledge by far there is no report on a colossal and long standing extra neural cysticercosis lesion in humans.
This report therefore is aimed at documenting a case of 56 year old female with a very rare gigantic solitary cysticercosis pseudo tumour of the neck for a period of quarter a century. Also alerts clinicians in endemic regions to consider cysticercosis as a differential diagnosis when evaluating patients with soft tissue lesions.
CASE REPORT
A 56 year old female who presented to our hospital with long standing history of a gradual but progressively growing left sided neck swelling for the past 25years.
Initially she was reluctant to seek medical attention, however with time the swelling became readily noticeable. This prompted her to start seeking medical intervention. Patient gave no history of concomitant significant constitutional symptoms. She grew up in a pastoralist family, with her parents rearing animals like pigs and goats. She does not use tobacco in any form.
General examination was unremarkable. However locally, she had a giant swelling occupying the left anterior and posterior triangles of the neck. The swelling was oval-shaped, well circumscribed, projecting out of the left anterior lateral aspect of the neck with longest transverse diameter stretching from midline of the neck, to the tip of the left shoulder.
The overlying skin was normal but fairly stretched compared to the surrounding skin. (Fig.1) The swelling was firm in consistency, non-tender and fixed to the underlying structures. No associated cervical lymphadenopathy was noted. The swelling moved with neither deglutition nor tongue protrusion. There was no palpable thrill or bruit on auscultation. ENT and other systemic examination were essentially normal.
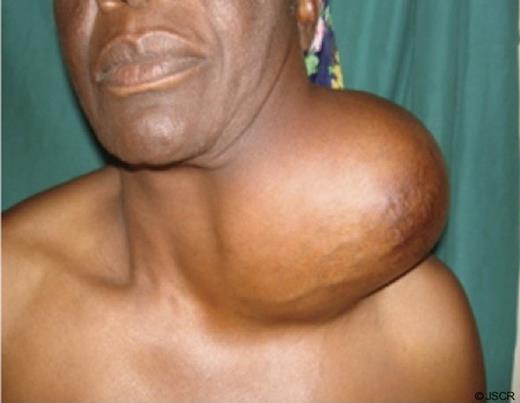
Gigantic cysticercosis pseudo tumour of the neck which had grown up gradually over decades.
Work-up of the patient comprised a battery of both specific and basic investigations. Specific investigations included Chest and cervical x-rays, Ultrasonography of the mass, Magnetic Resonance Imaging (MRI) of the brain, neck and incisional biopsy for histopathology examination.
The histopathology microscopic examination of the lesion demonstrated Tinea solium worms with multiple foci of dystrophic calcification and reactive plasma cellular infiltrate with extensive fibrosis, where as MRI ruled out brain involvement and clearly delineated the location, size and extent of the colossal cysticercosis lesion of the neck (Fig.2). Biochemical and haematological parameters were normal.
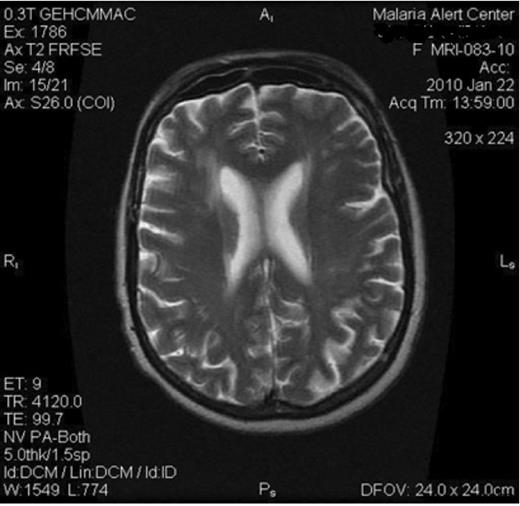
MRI of the brain revealed no masses which generally ruled out brain involvement (Neurocysticercosis)
In view of history, physical examination and investigations, surgery was deemed to be the most appropriate line of treatment at this stage. Therefore patient was planned for operation which was successfully done.
An extraordinary huge cysticercosis pseudo tumour of the neck was completely excised. Gross examination revealed a gigantic oval-shaped well capsulated pseudo tumour weighing 1.5 kg and measuring 10.1cm x 12.1cm x 14.5cm (Superior inferior x Anterior Posterior x Transverse) in size. The capsule wall thickness was 2.3cm. Cross sections of the mass revealed yellowish grey cheesy like areas together with multiple cystic areas (Fig 3). Patient did remarkably well post operatively and she had uneventful recuperation. (Fig.4)
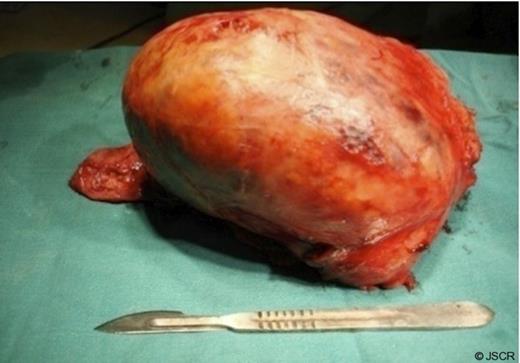
An extraordinary huge cysticercosis pseudo tumour weighing 1.5kg was completely excised.

Few weeks after surgery, generally patient had uneventful recuperation
DISCUSSION
Cysticercosis has been a well-known condition since antiquity. The earliest reports on tapeworms were cited in the work of ancient Egyptians far back to 2000 B.C. (2) Humans acquire cysticercosis when they ingest Taenia solium eggs either through faecal-oral route by eating faecally contaminated food or by auto infection. Ingestion of encysted pork may lead to intestinal infection of the adult tapeworm and a carrier state for the Taenia Solium eggs (3,4)
Tapeworm eggs hatch and embryos penetrate the intestinal wall and reach the blood stream where dissemination to different tissues occurs via systemic circulation. Sites where cysts may lodge include brain, spinal column, eyes, skeletal muscle and subcutaneous tissue (4). Encystment of the brain and spinal cord is life threatening and the most common manifestation, accounting for about 60% – 90% of all cases (1).
Specific investigations that can be employed in making diagnosis of cysticercosis include Computed Tomography (CT) scan, MRI and Ultrasonography (5-7). CT scan and MRI are useful in demonstrating the location, size and number of cysts. Occasionally pathognomic features of cysticercosis lesion like scolex or sucking parts of the larva may be demonstrated (8). Ultrasonography is sensitive for detection of ocular cysticercosis and may be used for guided Fine Needle Aspiration Cytology (FNAC). Generally radiological studies are mandatory to rule out central nervous system involvement (5-7).
Haematological profile often remains unaltered. Occasionally eosinophilia may be noted when there is leakage of parasitic antigen into surrounding tissues (3,5,6).
Serology can be done to detect the cysticercal antibodies in the serum or Cerebro Spinal Fluid. Biopsy from the lesion remains the gold-standard in providing a definitive diagnosis. Available treatment options for cysticercosis include antiparasitic therapy, antiseizure therapy, and surgery. Generally, treatment depends upon a number of factors such as location, size and number of cysts (5,6).
Surgery is feasible in cases of isolated intramuscular or subcutaneous cysticercosis lesions, which may otherwise require prolonged course of antiparasitic therapy. The case at hand is a classical paradigm. Antiparasitic therapy often comprises use of albendazole or praziquental together with steroids. Frequently antiepileptic medications are employed to control seizures especially in neurocysticercosis.
By and large cysticercosis is preventable, treatable and potentially eradicable disease entity. Conversely, delayed intervention may be associated with significant degree of morbidity and mortality.



