-
PDF
- Split View
-
Views
-
Cite
Cite
Kenneth Chan, Polly S Richards, Mike G Dilkes, Internal Carotid Artery Ectasia: The Value of Imaging Studies Prior to Biopsy of a Retropharyngeal Mass, Journal of Surgical Case Reports, Volume 2010, Issue 9, November 2010, Page 4, https://doi.org/10.1093/jscr/2010.9.4
Close - Share Icon Share
Abstract
The presence of retropharyngeal tissue mass often raises the suspicion of malignancy, especially in elderly patients. This prompts urgent biopsy to investigate tissue histology. We discuss a case where this is contraindicated as the retropharyngeal mass was illustrated by CT scanning and confirmed with MRI to be a tortuous coursing internal carotid artery. An awareness of this unusual anatomical variation and a careful interpretation of imaging studies both at the stage of differential diagnosis and pre-operative screening are essential to avoid damage to important structures, causing unnecessary complications.
INTRODUCTION
The examination of patients who present to an Ear, Nose and Throat (ENT) clinic with dysphagia involves flexible endoscopy via a transnasal route. On occasion, abnormalities are spotted within the postnasal space, and this raises the possibility of an occult nasopharyngeal cancer requiring a biopsy (1). We present a case where suspicious mass was incidentally found on Computed tomography (CT) scanning for other disease, but tissue biopsy would have caused unnecessary morbidity.
CASE REPORT
An 85 year old man was referred to the ENT/head and neck oncology clinic with a chronic cough and swallowing difficulty. He had a 5 year history of stage A chronic lymphoid leukaemia (CLL), which was stable and not requiring further therapy, and concurrent cutaneous T-cell lymphoma (CTCL). The CTCL had been managed with excision biopsy followed by Psoralen + UVA (PUVA) therapy. During the course of therapy he developed cutaneous recurrence at multiple sites, although this was static. Findings from physical examination of the neck were consistent with this history.
A CT scan, requested as part of his lymphoma follow-up, revealed asymmetrical fullness of the left nasopharynx due to a mass in the retropharyngeal space.(Figure 1) Owning to patient intolerance, nasoendoscopy was difficult in the clinic setting, and the nature of this swelling could not be properly determined. With the history of previous malignant disease, and the risk of recurrence or new disease being high, a biopsy was requested by the oncology team. However, since the CT imaging showed that the bulging mass could possibly be an artefact of a medially coursing left internal carotid artery (ICA), it was decided to perform a magnetic resonance imaging (MRI) prior to the biopsy. The MRI confirmed the ICA ectasia (often referred to as tonsillar loop) which manifested the asymmetry of the contour of the nasopharynx with prominence and fullness on the left just below the fossa of Rosenmuller.(Figure 2) There was no evidence of any mucosal abnormalities of nasopharynx or of the remainder of upper aerodigestive tract. No other pathological lesion was noted and the biopsy was cancelled.
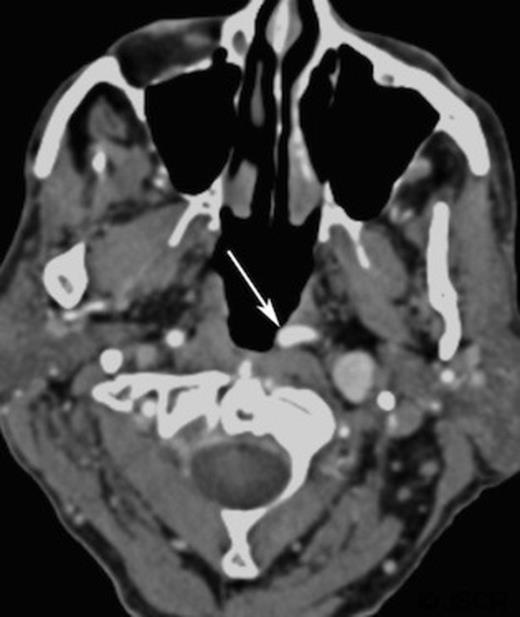
Contrast enhanced axial computed tomography of parapharyngeal region showing left retropharyngeal mass (arrow)
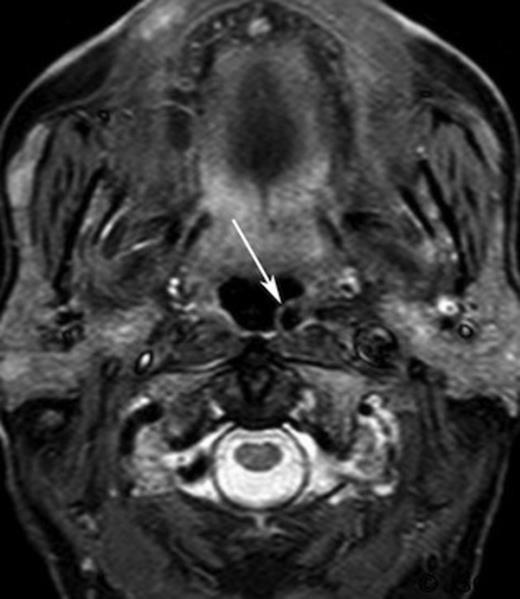
Short inversion time inversion recovery (STRI) axial magnetic resonance imaging of the retropharyngeal region (arrow)
DISCUSSION
The retropharyngeal space (RPS) is a narrow midline space extending from the skull base to upper mediastinum. The anterior and posterior boundaries of RPS are limited by the middle and deep layers of the deep cervical fascia, respectively. It usually contains only lymph node and adipose tissue, but could also be occupied by a tortuous ICA in rare cases (2). The cause of this vascular transposition is still unclear. It has been postulated that tonsillar loops occur during the eighth week of embryonic development, when caudal descent of dorsal aortic root into the chest should normally straighten the ICA (3).
Given the oncological background of this patient, malignancy was erroneously suspected on the CT scan. The differential diagnosis initially included retropharyngeal lymphadenopathy, mucosal lymphoma and nasopharyngeal carcinoma (4), and biopsy would be a logical investigation for defining the cell morphology and histological origin of the tissue mass (5). Should endoscopic examination have been possible, a pulsating appearance of the mass with intact mucosal lining may indicate its vascular nature. However, the ability to identify pulsation as part of naso-endoscopy is not widely accepted. In this case, non-invasive imaging was sufficient to recognise the anatomical abnormality and biopsy was averted.
In patients presented with unilateral mass with an intact mucosal lining, biopsy is still warranted to investigate suspected submucosal pathologies, particularly in someone with an active haematological cancer history, or someone of South-East Asian Chinese origin. However, careful analysis of CT or MRI imaging study is essential for identifying ICA ectasia and should be performed as a safety measure at the initial stage prior to biopsy, which is good clinical practice anyway, to avoid biopsy artefact in patients who subsequently are shown to have proven tumours.



