-
PDF
- Split View
-
Views
-
Cite
Cite
Wassim Abi Jaoude, Christopher Lau, Gainosuke Sugiyama, Albert Duncan, Management of Ampullary Carcinoid Tumors with Pancreaticoduodenectomy, Journal of Surgical Case Reports, Volume 2010, Issue 8, October 2010, Page 4, https://doi.org/10.1093/jscr/2010.8.4
Close - Share Icon Share
Abstract
A 66 year old female was found to have an ampullary mass on endoscopic examination. A pancreaticoduodenectomy was performed and the pathology was consistent with carcinoid tumor. Carcinoid tumors of the ampulla of Vater are rare tumors of the gastrointestinal tract, accounting for 0.3-1% of gastrointestinal carcinoids. Management of ampullary carcinoid tumor with pancreaticoduodenectomy is in accordance with current recommendations.
INTRODUCTION
Carcinoid tumors of the ampulla of Vater are very rare tumors, accounting for 0.3 to 1 % of gastrointestinal carcinoids. To date, less than 110 cases have been published, mostly in the form of case reports.(1) Large studies are lacking and therefore the management of these tumors is still controversial. Most authors recommend pancreaticoduodenectomy, although local resections are being proposed more frequently for selected cases.(2)
We report a case of ampullary carcinoid and review the literature on the surgical management of these rare tumors.
CASE REPORT
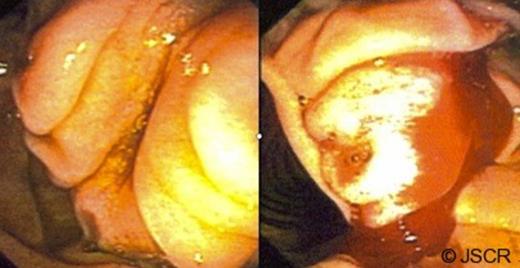
A 66 year-old woman was referred to the surgeon’s office when she presented with a five month history of upper abdominal pain and diarrhoea. A CT scan of the abdomen and pelvis obtained upon presentation to the emergency department showed intrahepatic and extrahepatic bile duct dilatation. There were no masses in the cystic bile duct (CBD) or the pancreas. This was followed by an oesphago-gastro-duodenoscopy (OGD) that showed a prominent ampulla (Figure 1) with very hard tissue suspicious for malignancy. On oesophageal ultrasound, there was a submucosal mass, isoechoic, not invading the muscularis propria (Figure 2), and without involvement of the pancreas. There were no enlarged lymph nodes. The biopsy specimen was positive for a focal carcinoid tumor on a background of duodenitis. The cells stained positive for Chromogranin, Synaptophysin and Cytokeratin.

A complete metastatic work-up was then conducted including serum markers (serotonin, Chromogranin A, urine 5-HIAA) and a total body octreotide scan, which were negative.
The patient was admitted for an elective pancreaticoduodenectomy. Her preoperative physical exam and laboratory tests were unremarkable. A formal pancreaticoduodenectomy was performed with an end-to-end pancreaticojejunostomy, end-to-side choledochojejunostomy and an antrectomy with gastrojejunostomy. Two Jackson-Pratt drains were left in place next to the choledochojejunal and the pancreaticojejunal anastomoses. The procedure was completed without complications.
The pathology report revealed a 3.5 cm low grade neuroendocrine carcinoma invading into the duodenum and focally compressing the CBD (Figure 3). One of five peripancreatic lymph nodes was positive for metastatic disease. The perigastric lymph nodes were negative for malignancy. The tumor stained positive for chromogranin, synaptophysin and neuron specific enolase.

DISCUSSION
Carcinoid tumors have an incidence of 1.6-2 cases per 100000 persons per year making ampullary carcinoids extremely rare.(2) There are a total of 105 cases reported to date in the literature.(1) Compared to duodenal and other carcinoid tumors, ampullary carcinoids involve a younger population with a mean age at diagnosis of 51 years (23-78 years). The male to female ratio is 2 to 1. (3)
The most common symptom in carcinoids of the ampulla of Vater is jaundice (53.1-62%) compared to abdominal pain and reflux for duodenal carcinoids. Non specific abdominal discomfort (24%) is the second most common symptom with gastrointestinal bleeding and pancreatitis (6%) being less frequent. 4-10% of patients will experience weight loss (1). An association with Von Recklinghausen Neurofibromatosis is present in up to 26% of cases.(3,4)
The preoperative diagnosis of ampullary carcinoids is correct in only 14% of cases. Ampullary carcinoids are submucosal tumors with ulceration of the mucosa occurring in only 6% of cases and therefore the yield of the biopsies is low. The most helpful diagnostic techniques is OGD and ERCP.(3,5) The adjunct of endoscopic ultrasound can be helpful in detecting the depth of invasion and the presence of lymph node metastases. The role of MRI in this field is still controversial and the literature in this regard is limited. CT scan and transabdominal ultrasound are less accurate modalities for diagnosis of the primary lesion, although computed tomography is useful in detecting metastases. Total body octreotide scans can also be used in the metastastic work-up (5) and most recently radionucleotide scanning such as MIBG scintiscan is playing an important role.
Serum markers can be useful in diagnosis. Ampullary carcinoid cells express chromogranin in 92% of cases and neuron specific enolase, synaptophysin and cytokeratin in 100%; somatostatin is found in 58 to 67% of cases. Serotonin is secreted in 17% of cases as well as CCK. 25% of tumors stain positive for insulin and 13% are negative for hormonal staining. (3)
Given the relatively younger age of the patients, the lack of reliability of preoperative staging and the concern for incomplete tumor removal, most authors recommend treatment with a pancreaticoduodenectomy.(4) However, a more limited resection and even endoscopic excision can be considered in small mobile tumors, tumors less than 2 cm in the absence of nodal involvement, tumors limited to the submucosa, and in high surgical risk patients.(3-4) Alternatives to pancreaticoduodenectomy include transduodenal ampullectomy, retroduodenal resection of the ampulla and pancreas preserving duodenectomy.
Despite their more aggressive behavior compared to duodenal carcinoids, ampullary carcinoids have a good prognosis, with a five year survival of 90%. Only about 6% die from progessive or metastatic disease.(3) The stage of the tumor (as defined by the TNM classification of the ENETS –European Neuroendocrine Tumor Society) has no prognostic impact. However, high grade tumors are associated with a worse prognosis as compared with low grade tumors making histologic grade a better predictor of survival.



