-
PDF
- Split View
-
Views
-
Cite
Cite
Faisal Alsaleh, Abdullah Aljarbou, Mohammed Bin Shunayf, Yazeed Alghtani, Faisal Altwijri, Abdullah Alturki, Suprapubic catheter insertion complicated by small bowel obstruction requiring laparotomy: a case report, Journal of Surgical Case Reports, Volume 2026, Issue 1, January 2026, rjaf1006, https://doi.org/10.1093/jscr/rjaf1006
Close - Share Icon Share
Abstract
Suprapubic catheterization (SPC) is a common minimally invasive procedure with various urological indications. However, rare complications like bowel obstruction can occur, causing serious consequences. We report a case of a 70-year-old female who developed bowel obstruction 10 days after SPC insertion. Imaging confirmed the diagnosis and exploratory laparotomy revealed bowel obstruction caused by an adhesive band covering the terminal ileum, which was successfully released. This case highlights the importance of precise catheter insertion techniques, early recognition of complications, and prompt intervention to improve patient outcomes. Continued case reporting is essential to improve awareness and guide best practices for such complications.
Introduction
Suprapubic Catheterization (SPC) is a widely performed procedure with various indications, including acute urinary retention in the emergency setting if urethral catheterization is difficult or dangerous, chronic urinary retention, urethral trauma, and palliation [1].
It is typically regarded as a safe and minimally invasive procedure. However, complications such as bowel injury or obstruction, though rare, can have significant clinical implications. These complications often arise due to the close anatomical relation between the bladder and surrounding structures, particularly the bowel.
This report presents a rare case of small bowel obstruction after SPC placement, which emphasizes the importance of heightened vigilance during the procedure as well as the need for timely diagnosis and management of this serious complication.
Case presentation
A 70-year-old female with a past medical history of diabetes mellitus, hypertension, dyslipidemia, hypothyroidism, and a stroke in 2019 resulted in a neurogenic bladder for which she underwent suprapubic catheter insertion. Her surgical history was only notable for a prior cesarean section.
The patient presented to the Emergency Department ten days after the SPC insertion with a three-day history of abdominal pain, vomiting, and obstipation. Physical examination revealed abdominal tenderness and distention. The SPC was noted to be draining clear urine. Her vital signs showed elevated blood pressure (159/69 mmHg); otherwise, she was vitally stable. Laboratory findings were notable for hyponatremia (115 mmol/L).
A computed tomography (CT) scan of the abdomen and pelvis was performed for further evaluation. The coronal view demonstrated a markedly distended stomach, mesenteric fat stranding with a small amount of free fluid, along with bowel dilation involving the mid and proximal small bowel loops (measuring up to 4 cm) with a transition zone at the site of bowel twisting over the suprapubic catheter (Fig. 1). On the sagittal view, the suprapubic catheter was seen positioned correctly within the bladder (Fig. 2). The bowel demonstrated normal enhancement, with no evidence of wall thickening, pneumatosis intestinalis, or pneumoperitoneum.
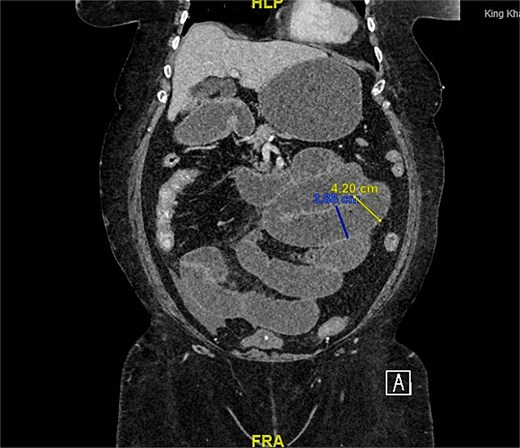
CT scan coronal view: Demonstrating distended small bowel loops consistent with small bowel obstruction, with a transitional zone at the twist of bowel over the suprapubic catheter.
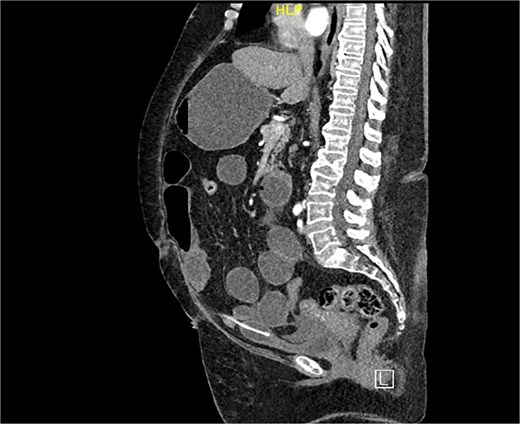
CT scan sagittal view: Demonstrating suprapubic catheter in its appropriate position within the bladder.
The patient was admitted and started on intravenous fluids as she could not tolerate oral intake; antiemetics and antibiotics were administered as well. A Foley catheter and nasogastric (NG) tube were inserted, and the suprapubic catheter was removed. She was managed conservatively for four days without improvement. Consequently, the patient was taken to the operating room for an exploratory laparotomy. Intraoperatively, while running the bowel, an adhesive band around the terminal ileum was found covering the small bowel, leading to significant proximal bowel dilation. The adhesive band was released, resulting in distal bowel collapse, which indicated resolution of the obstruction. A small serosal tear (<1 cm) at the site of the band was identified and repaired with interrupted seromuscular sutures. Upon re-running the bowel, hard stools were palpated in the colon, for which a trial of bowel milking was performed. The nasogastric tube was connected to suction and used to help evacuate bowel contents.
Postoperatively, the patient progressed well without complications. Prior to discharge, a new SPC was successfully inserted into the correct position by interventional radiology under ultrasound guidance to avoid further complications. The patient tolerated a regular diet and was discharged home in stable condition.
Discussion
Despite being a relatively simple procedure, suprapubic catheterization carries some risks. A 2006 study conducted in the UK identified recurrent urinary tract infections (21%) and catheter blockage (25%) as the most common long-term issues, with an associated mortality rate of 1.8% [2]. Bowel obstruction, however, remains one of the rarest complications, with only 12 cases found in the literature [3–5], for which this condition might be overlooked due to its rarity. A review of the literature indicates that bowel obstruction following suprapubic catheterization can present anywhere from 1 day to as long as 4 years post-procedure, with average age of affected patients being 75.88 years [3]. The mechanism of injury can be caused by the SPC placement leading to direct bowel injury or due to subsequent adhesions leading to obstruction.
Patients usually present with symptoms of small bowel obstruction, which include acute abdominal pain, vomiting, electrolyte imbalances, and metabolic alkalosis. Abdominal distension is common, particularly with high or complete obstructions, and it is due to the accumulation of gas and fluids above the obstruction. Changes in bowel movements, such as obstipation may be observed [6]. As for confirming the diagnosis of bowel obstruction, CT imaging has been proven to be highly diagnostic, and it is frequently used in such cases [7].
11 cases of small bowel obstruction secondary to suprapubic catheter were managed surgically [3, 4], with only one case managed conservatively [5]. Laparotomy remains the standard treatment for small bowel obstruction in most cases, particularly in cases of complete obstruction, strangulation, or perforation. In our case, the patient was managed conservatively for 4 days without improvement. Therefore, a laparotomy was indicated to relieve the obstruction. Post-operatively, the patient progressed well without any complications.
Regarding the preventive measures during suprapubic catheter insertion, proper patient positioning, particularly placing the patient in a Trendelenburg position, can help minimize the risk of bowel injury by shifting intra-abdominal contents away from the insertion site [8]. Additionally, the British Association of Urological Surgeons (BAUS) considers ultrasound use to be helpful in patients with a surgical history to mitigate bowel injury, although there is a lack of sufficient evidence to confirm its reliability [1].
Healthcare providers should maintain awareness of this rare complication, ensuring timely and effective care to minimize adverse outcomes, as early recognition is essential to ensure timely diagnosis to mitigate morbidity.
Conclusion
In conclusion, small bowel obstruction is considered a rare yet significant complication following suprapubic catheter insertion. This case brings attention to the need to use careful technique and have anatomical awareness during catheter insertion to reduce the occurrence of this complication. Additionally, it emphasizes the importance for healthcare providers to consider bowel-related complications in patients presenting with abdominal symptoms after suprapubic catheter placement, as early detection and management can optimize patient outcomes. Furthermore, it highlights the need for continued reporting of similar cases to improve awareness and guide best practices regarding this complication.
Acknowledgement
The authors have no acknowledgements to declare.
Author contributions
Faisal Alsaleh - Manuscript editing, Manuscript revision, Supervision. Abdullah Aljarbou - Final approval of the manuscript, Supervision. Mohammed Bin Shunayf - Literature review, Manuscript drafting, Correspondence. Yazeed Alghtani - Literature review, Manuscript drafting. Faisal Altwijri - Data collection, Manuscript editing. Abdullah Alturki - Data collection, Manuscript editing.
Conflict of interest statement
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Funding
No external funding was received.
Data availability
Data are available upon reasonable request.
References
Schick MA, Kashyap S, Collier SA, et al. Small Bowel Obstruction. 2025 Jan 19. In:
Corder CJ, LaGrange CA. Suprapubic Bladder Catheterization. 2022. In:



