-
PDF
- Split View
-
Views
-
Cite
Cite
Chrystal Calderon, Nishana Singh, Vanessa Ramoutar, Kavita Doodnath, Devindra Ramnarine, A rare case of posterior fossa collision tumor involving low-grade astrocytoma and meningioma, Journal of Surgical Case Reports, Volume 2025, Issue 9, September 2025, rjaf770, https://doi.org/10.1093/jscr/rjaf770
Close - Share Icon Share
Abstract
This case highlights a rare phenomenon, of two benign tumors, a low-grade astrocytoma, and meningioma, occurring simultaneously in the infratentorial compartment. This unique case seeks to add to the current literature on collision tumors. A 25-year-old female presented with a 9-month history of neck pain and right arm weakness. Imaging demonstrated a ring-enhancing cystic lesion in the posterior fossa, with solid enhancing extension into the spinal canal. The main differential diagnosis was an ependymoma. A suboccipital craniotomy, C1 laminectomy and C2–C4 laminoplasty, was performed and revealed two distinct tumor entities. Histopathology revealed that the cerebellar component was consistent with a low-grade astrocytoma and the extra-axial component was a meningioma. Coexisting tumors of different cell lineage and distinct borders, collision tumor, are very uncommon in clinical practice, with most cases diagnosed intra and post-operatively. A complete medical and genetic assessment is critical for the holistic management of these patients.
Introduction
Primary posterior fossa tumors in the adult population are relatively uncommon compared to the pediatric age group. Hence, varied tumor patterns can be seen in these distinct populations [1, 2]. In the adult population, differentials include both primary and secondary space occupying lesions. Some primary lesions occurring in the posterior fossa compartment include astrocytomas and meningiomas. However, these are typically less common in the infratentorial region when compared to the supratentorial. More so, these coexisting tumor pathologies, in the absence of risk factors that may increase the propensity for tumor growth, such as a known underlying neurocutaneous disorder or previous radiation therapy, are seldom recognized [3, 4].
The term, collision tumor, best describes this phenomenon of a lesion with two or more discrete cell lineages, having a defined border between them [5]. This is a unique neurosurgical phenomenon, and this case report highlights this occurrence. The underlying pathogenesis has not been ascertained, with several coexisting theories, such as coincidence, malignant transformation, and possible external inciting factors. The presence of these two distinct primary brain tumors, an astrocytoma and meningioma, occurring simultaneously in this part of the brain, the posterior fossa, is indeed rare.
Case report
A 29-year-old female with a history of undifferentiated connective tissue disorder presented to the outpatient setting with a 9-month history of progressively worsening neck pain and weakness of the right arm. This was associated with intermittent paresthesia of the right arm. There was no past medical history of neurocutaneous disorders, prior radiation therapy, or significant family history. Her initial neurological examination was normal except for decreased power in the right upper limb, Medical Research Council Grade 4+/5 and positive Babinski and Hoffman’s reflexes bilaterally. No sensory deficits were appreciated.
Magnetic resonance imaging brain with gadolinium demonstrated a ring enhancing cystic lesion in the posterior fossa, with solid enhancing extension into the spinal canal down to the C3 level (Fig. 1). The radiological appearance was consistent with an ependymoma.
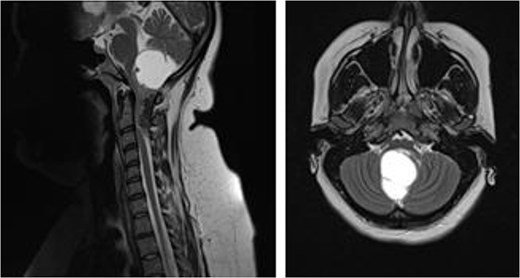
MRI brain demonstrating cystic posterior fossa mass, with solid component extending past the foramen magnum, down to the level of C3, on sagittal and axial views, respectively.
A scheduled suboccipital craniotomy, C1 laminectomy and C2–C4 laminoplasty, was performed. Intra-operatively two distinct, separate lesions were identified. An extra-axial tumor and an intrinsic cerebellar mass with invasion into the underlying brainstem was noted (Fig. 2). There were clear pial margins between both lesions. Gross total resection was achieved for the extra-axial mass and a subtotal resection was achieved for the intra-axial cerebellar component. A subtotal resection was secondary to the high risk of injury to adjacent structures and intra-operative bradycardia noted as surgical resection progressed (Fig. 3). This patient had an uneventful post-operative course and had no neurological deficits.
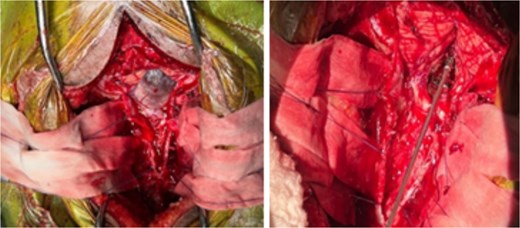
Intra-operative photography demonstrating cystic component and solid components of tumor pathologies, cyst intact, and cyst aspirated, respectively.
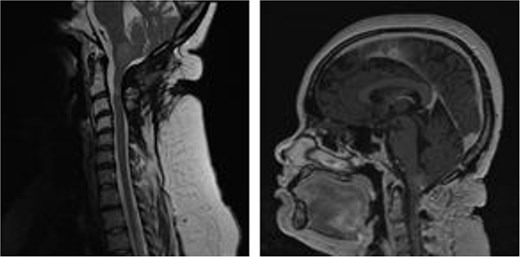
MRI brain with gadolinium, sagittal views T2- and T1-weighted, respectively, demonstrating partial resection of cystic, intra-axial component and complete resection of solid, and extra-axial component of tumor.
Histopathology diagnosis confirmed that the intra-axial lesion was consistent with a low-grade astrocytoma. This was supported by immunohistochemistry performed on the sample of the intra-axial lesion, this demonstrated positive glial fibrillary acidic protein, negative epithelial membrane antigen, and a Ki-67 < 1% positivity. The extra-axial component was consistent with a WHO Grade 1 psammomatous meningioma (Fig. 4). Following a multidisciplinary team assessment, radiotherapy was advised and completed. Genetic testing was performed and confirmed the absence of any underlying neurocutaneous genetic disorders.
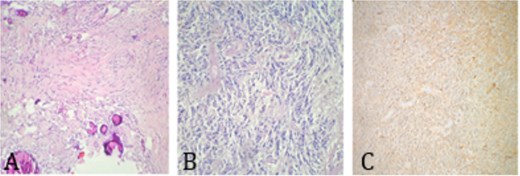
Histology imaging demonstrating. (A) Psammomatous meningioma with cellular whorls and psammoma bodies; no atypia or mitoses. (B) Low-grade glioma—a hypercellular tumor composed of glial cells with mild atypia; no necrosis and no mitosis. (C) GFAP positivity in low-grade glioma.
Discussion
This case report on intracranial collision tumor seeks to add to existing literature on this rare neurosurgical occurrence, highlighting the challenges in clenching a diagnosis and managing these complex cases. The presence of multiple coexisting brain tumors of varied cell lineages is commonly noted when an accompanying risk factor is present. This includes underlying neurocutaneous disorders, other genetic abnormalities, and previous history of radiation therapy [3, 4]. This is easily identifiable with the common inheritable phakomatoses of neurofibromatosis Type 1 and 2 [6, 7]. More so, neurofibromatosis Type 2 may be linked with the presence of schwannomas, meningiomas, and ependymomas in its diagnostic algorithm [6]. In this case patient, radiological assessment was misinterpreted as the more common single posterior fossa tumor pathology, an ependymoma. The diagnosis of two varied tumors was only suspected intra-operatively and confirmed on histopathology. Furthermore, there were no significant clinical features in her past medical history that would increase suspicion of otherwise. Therefore, post-operatively, further medical assessments of this patient were important to rule out any undiagnosed genetic disorders.
There have been several cases of collision tumor of the central nervous system, with varied tumor combinations reported [3, 8–10]. One literature review highlighted this clinical entity, and included reported cases of gliomas and meningiomas, all involving the supratentorial region [3]. None of the cases portrayed in this research article involved the posterior fossa region, further depicting how uncommon this case patient is [3]. The exact underlying pathophysiology of this clinical phenomenon has only been postulated. One of these explanations includes a primary tumor inciting tumorigenesis in nearby tissue through varied growth factor alterations [3, 9, 11]. Others entertain the role of genetic abnormalities and the possibility of coincidental random occurrence [3, 8]. This leaves much to consider in terms of these tumor presentations. It has been reported that the combination of meningioma and glioblastoma multiforme to be the most prevalent primary collision tumor [3, 11]. Our case differs, with two low-grade pathologies being identified.
When dealing with any complex posterior fossa tumor, especially when two differing pathologies coexist, surgical planning in a multidisciplinary team setting is essential. In this case, the diagnosis of collision tumor was only suspected on observation of the operative site. However, the surgical goal was not altered, which was an attempt at a maximal safe resection, of the two primary brain tumors. A gross total resection was attempted for the cerebellar component, but the patient did become bradycardic intra-operatively, and hence a subtotal resection was attained for the intrinsic glioma. The clinical management of collision tumors is atypical, and a suggested standard of care has not been established. Attempts at a gross total resection once safe to do so is advocated [3]. Due to the rare nature of collision tumors, case reports, although limited in its research value, help in gaining insight into these surgically challenging pathologies.
In this clinical case, the patient had no clear signs, family history, or genetic alterations pointing to a neurocutaneous disorder or genetic syndrome. Additionally, given the proximity of the two primary tumors in a confined space, differentiation as two separate tumors was not elucidated on radiological imaging. Holding on to key surgical techniques will drive a successful operative outcome.
Conclusion
Collision tumor, low-grade astrocytoma and meningioma, in the posterior fossa is extremely rare. Especially in the setting of no significant risk factors to explain these coexisting tumors. These cases are not easily identifiable pre-operatively, making their surgical management even more arduous. This case was surgically managed with a maximal safe resection of the two primary brain tumors, with a good prognostic outcome.
Conflict of interest statement
None declared.
Funding
None declared.
Consent
Informed consent was attained.
Ethical approval
Ethical approval is exempt in this case report publication. Informed written consent has been attained.



