-
PDF
- Split View
-
Views
-
Cite
Cite
Sehar Shahid, Kuda Galketiya, Optimizing sentinel lymph node detection in melanoma: the value of dual tracer techniques in unpredictable drainage patterns, Journal of Surgical Case Reports, Volume 2025, Issue 9, September 2025, rjaf764, https://doi.org/10.1093/jscr/rjaf764
Close - Share Icon Share
Abstract
Sentinel lymph node biopsy plays a vital role in staging and treatment planning for patients with melanoma. We describe the case of a 54-year-old man with a primary melanoma on the lower back, where preoperative lymphoscintigraphy revealed drainage to both the expected inguinal region and the axilla. This case illustrates the practical value of using both blue dye and scintigraphy to guide sentinel node identification, especially when lymphatic drainage patterns are less predictable.
Introduction
Melanoma is an aggressive skin cancer with a high potential for lymphatic spread. Sentinel lymph node biopsy (SLNB) provides crucial prognostic information and guides decisions about further management. Typically, SLNB is considered when the Breslow thickness exceeds 1 mm. The most used methods for identifying sentinel nodes include blue dye and radiotracer (scintigraphy). While either method can be used alone, combining both increases detection sensitivity and reduces the risk of missing involved nodes. One key advantage of scintigraphy is its ability to detect drainage pathways that may not align with what would be expected from the tumors’ location.
Case report
A 54-year-old man presented with a pigmented lesion on his right lower back that had gradually increased in size. Excision biopsy confirmed malignant melanoma with a Breslow thickness of 2.1 mm and a close peripheral margin of 0.5 mm. At a multidisciplinary oncology meeting, a decision was made to proceed with a wide local excision and SLNB.
Preoperative lymphoscintigraphy was performed to detect the sentinel lymph node (Fig. 1), expecting it to be in the right inguinal region (Fig. 2). However, drainage to both the right axillary (Fig. 3) and inguinal areas was demonstrated. During surgery, a gamma camera confirmed drainage to both regions (Fig. 4). Blue dye was injected around the previous scar, and sentinel nodes were dissected guided by both blue dye and gamma camera for histopathology.
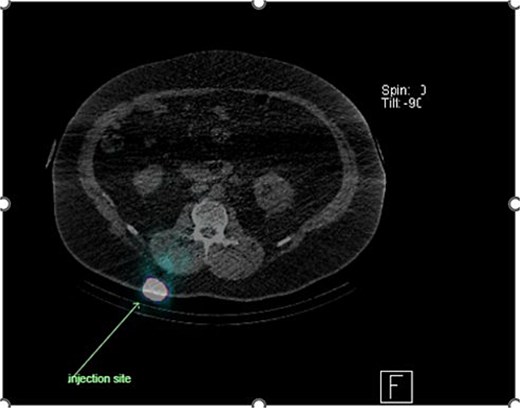
Lymphoscintigraphy showing drainage from the right lower back lesion.
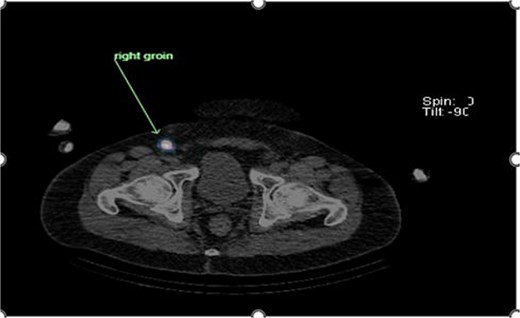
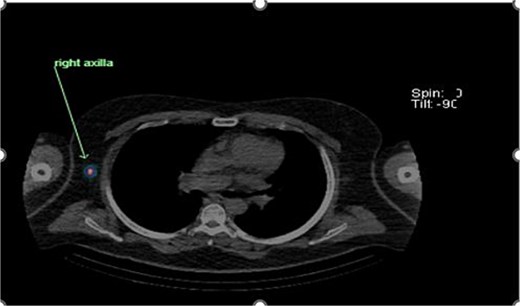
Unexpected drainage visualized toward the right axillary lymph nodes.

Intraoperative gamma probe confirming dual drainage to axillary and inguinal regions.
Histology showed no residual malignancy in the re-excision specimen. The right axillary node showed involvement by metastatic melanoma, while the groin lymph node was negative.
A decision for adjuvant therapy with BRAF (B-Raf proto-oncogene, serine/threonine kinase involved in the MAPK/ERK pathway and frequently mutated in melanoma)/MEK (mitogenactivated protein kinase kinase, a downstream target in the MAPK/ERK pathway) inhibitors was made following discussion at multidisciplinary meeting.
Discussion
SLNB is used in melanoma staging in selected patients depending on factors including Breslow thickness. Sentinel lymph node metastasis is a key prognostic factor and influences adjuvant therapy decisions [1]. SLNB has led to a reduction in unnecessary lymph node dissection and associated morbidity. It has become standard in surgical treatment of melanoma, breast, cervical, and vulvar cancers [2, 3].
Sentinel node identification typically involves peritumoral injection of blue dye and radioisotopes. Most studies indicate that using both techniques increases sensitivity and specificity [4]. With blue dye alone, dissection is performed in the area where drainage is expected. Scintigraphy, however, allows for a full-body scan to detect unexpected drainage sites. A gamma probe is used during surgery to localize labelled lymph nodes, which are then excised and examined histologically [5].
Scintigraphy provides a clear advantage by detecting sentinel nodes outside of expected drainage pathways. There are reported cases in breast cancer where sentinel nodes were identified in the ipsilateral axilla despite previous surgeries [6, 7].
In our patient, the groin was the expected site of drainage. However, scintigraphy demonstrated dual drainage, and the axillary node was found to be involved.
Although newer agents like indocyanine green (ICG) are being studied for SLNB, they are not yet widely available, especially in regional settings. Blue dye remains a practical and accessible tool that still holds value in combination with scintigraphy. Trials support ICG use, but accessibility remains a limiting factor [8].
This case reinforces the importance of not assuming drainage patterns based on tumor location alone. SLNB relies on anatomy, sound surgical technique, and the coordinated effort of a multidisciplinary team.
Conclusion
Scintigraphy plays a critical role in identifying sentinel nodes in atypical drainage patterns. When combined with blue dye, it enhances the accuracy of staging and guides appropriate treatment [9].
Conflict of interest statement
None declared.
Funding
None declared.
Patient consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.



