-
PDF
- Split View
-
Views
-
Cite
Cite
Wejdan M Alresheedi, Mohammed S Alfehaid, The diagnostic journey: right groin swelling in a young female revealing canal of Nuck hydrocele, Journal of Surgical Case Reports, Volume 2025, Issue 9, September 2025, rjaf727, https://doi.org/10.1093/jscr/rjaf727
Close - Share Icon Share
Abstract
Canal of Nuck hydrocele represents a rare anatomical entity in female patients and is predominantly documented in pediatric populations. This condition arises from incomplete obliteration of the processus vaginalis during embryogenesis. A 23-year-old female presented with a 3-week history of right groin pain and swelling. Physical examination revealed a small right inguinal swelling with a positive cough impulse. Subsequent imaging demonstrated a cystic lesion extending through the right inguinal canal without evidence of bowel or omental herniation. The patient underwent elective diagnostic laparoscopy with hydrocelectomy and mesh hernioplasty. The postoperative course was uneventful with complete symptom resolution and benign histopathological findings. This case contributes to the growing literature documenting adult presentations of canal of Nuck hydrocele. Our findings suggest that this condition should be included in the differential diagnosis of inguinal masses in adult females. The successful management through laparoscopic approach demonstrates the efficacy of this minimally invasive surgical strategy.
Introduction
Canal of Nuck hydrocele represents a rare anatomical entity in female patients, first described by Dutch anatomist Anton Nuck in 1691 [1]. While predominantly documented in pediatric populations, recent literature suggests increasing recognition of adult cases, potentially attributed to expanded utilization of cross-sectional imaging over the past three decades [1, 2]. This condition arises from incomplete obliteration of the processus vaginalis, which normally occurs during the first year of life [2]. We present a case of canal of Nuck hydrocele in a young adult female, highlighting the diagnostic approach and surgical management of this uncommon condition.
Case presentation
A 23-year-old nulliparous female with no significant medical history was referred from the Obstetrics and Gynecology department to General Surgery, presenting with progressive right groin pain and swelling of 3 weeks’ duration. The pain was characterized as dull, localized to the right inguinal region without precipitating factors. She denied alterations in bowel habits, fever, vomiting, or prior herniation history.
Physical examination revealed a well-developed female in no acute distress. Abdominal examination demonstrated a soft, non-distended abdomen without palpable defects. Notable findings included a small right inguinal swelling extending inferiorly to the ipsilateral labium majus, with positive cough impulse that became more prominent when standing. The overlying skin remained intact. No inguinal lymphadenopathy was appreciated, and genitourinary examination was unremarkable.
Laboratory studies, including complete blood count and comprehensive metabolic panel, were within normal limits. Initial ultrasonography (US) revealed an oblong cystic lesion with fine septations, measuring 6.5 × 3 cm, extending through the right inguinal canal into the labium majus (Figs 1 and 2). Subsequent pelvic magnetic resonance imaging (MRI) corroborated these findings, demonstrating a right lower abdominal cystic lesion with thin septations extending to the inguinal region, showing low T1 and high T2 signal intensity, measuring ~7 × 3.5 cm (Figs 3 and 4). No evidence of bowel or omental herniation was observed, suggesting canal of Nuck hydrocele.

US of the right inguinal area showing oblong cystic lesion measuring 6.5 × 3 cm, extending through the right inguinal canal into the labium majus (arrow).
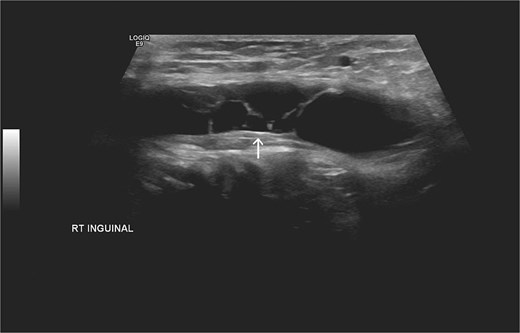
Additional US of the right inguinal area showing fine internal septations of the lesion as indicated by the arrow.
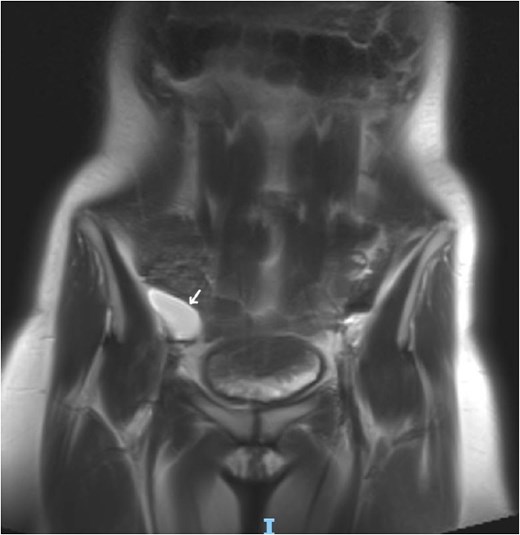
Coronal MRI view of the pelvis, showing well-defined cystic lesion with low T1 and high T2 signal intensity, measuring ~ 7 × 3.5 cm (arrow).

Axial MRI view of the pelvis, showing the extension of the cyst into the right inguinal canal with no bowel or omental herniation (arrow).
The patient underwent elective diagnostic laparoscopy with hydrocelectomy and mesh hernioplasty. Surgical technique included placement of a 5-mm supraumbilical camera port via open technique with pneumoperitoneum establishment. Two additional working ports were placed bilaterally in the lower abdomen under direct visualization. Diagnostic laparoscopy revealed minimal hemoserous peritoneal fluid and prominent right inguinal swelling confirming the encysted hydrocele (Video 1 and Fig. 5). The peritoneal cavity appeared otherwise unremarkable. A peritoneal flap was created in the right inguinal region, the preperitoneal space was explored, and the encysted hydrocele was carefully dissected and excised without rupture (Fig. 6). The right inguinal region was reinforced with anatomical mesh, and the peritoneal flap was closed.
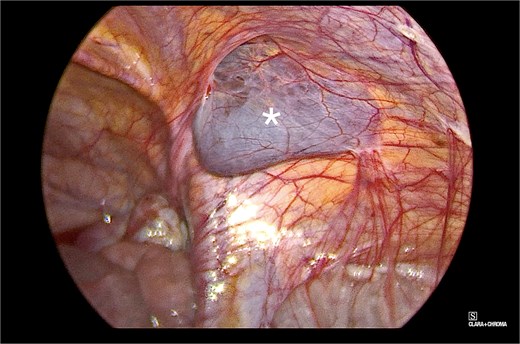
Intraoperative view of the right inguinal area, demonstrating a bluish-gray, fluid-filled sac (marked with an asterisk in the image). The surrounding structures appeared normal and showed typical anatomy.
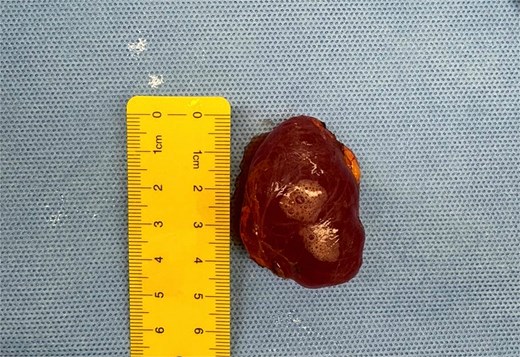
Intraoperative finding showing the excised specimen, which was fluid-filled and reddish-brown in color with smooth, glossy appearance.
Histopathological examination revealed a benign peritoneal inclusion cyst with no malignancy, consistent with canal of Nuck hydrocele. The patient’s postoperative course was unremarkable with same-day discharge. Two-week follow-up demonstrated satisfactory wound healing without complications. One-month assessment revealed complete resolution without recurrence, and the patient resumed normal activities. Written informed consent was obtained for publication.
Discussion
Canal of Nuck hydrocele illustrates the relationship between embryological development and subsequent pathology [3]. During embryogenesis, around the twelfth week of gestation, the processus vaginalis accompanies the round ligament through the inguinal canal in females [2, 4]. Under normal circumstances, obliteration begins around the seventh month of gestation and achieves complete closure within the first year after birth [3, 5]. When this obliteration process fails, the persistent processus vaginalis becomes known as the canal of Nuck [3], which can give rise to various pathological conditions [2]. Hydrocele represents the most commonly encountered pathology, developing when an imbalance occurs between fluid secretion and absorption by the mesothelial lining [4]. This dysregulation may be triggered by inflammation, trauma, or impaired lymphatic drainage, leading to fluid accumulation within the patent canal [6]. Other potential pathologies include hernia, infection, ectopic gonads, endometriosis, benign tumors, and rarely, malignant neoplasms [2]. Three distinct anatomical variants have been described. Type 1 develops when the proximal portion obliterates while fluid accumulates distally, creating an encysted hydrocele that presents as a non-compressible mass unaffected by Valsalva maneuvers. Type 2 maintains communication with the peritoneal cavity due to complete patency, typically presenting as reducible swelling that varies with intra-abdominal pressure. Type 3 combines features of both variants, displaying an hourglass configuration due to constriction at the deep inguinal ring [4, 7].
While traditionally considered a pediatric condition, adult presentations are increasingly recognized [3]. Clinical manifestations typically include inguinal and/or labial swelling, often accompanied by varying degrees of discomfort [8]. US has emerged as the principal diagnostic modality due to its efficiency in differentiating hydrocele from other inguinal pathologies [2, 9, 10]. Sonographic findings typically reveal anechoic or hypoechoic, well-circumscribed cystic lesions without internal vascularity on Doppler examination [9, 11]. Our case demonstrated the classic appearance of an oblong cystic lesion with fine septations. When additional tissue characterization is required, MRI provides superior soft tissue detail, confirming the cystic nature of the lesion [12]. In our patient, MRI served as second-line imaging, offering excellent delineation while excluding bowel or omental herniation. However, CT remains valuable when herniation is suspected [5]. Initial US findings characterized the lesion and guided subsequent MRI evaluation [1].
Surgical exploration with histopathological confirmation remains the gold standard for diagnosis [11, 13]. The choice of surgical approach should be individualized based on extent of pathology, diagnostic certainty, coexisting conditions, surgeon expertise, and patient factors [5]. Laparoscopic techniques offer enhanced visualization, improved cosmetic outcomes, shorter hospitalization, and reduced postoperative morbidity [13]. Our management utilized laparoscopic assessment followed by hydrocelectomy and mesh hernioplasty [13].
This case adds to the growing literature documenting adult presentations of canal of Nuck hydrocele. Although rare, our findings suggest that this condition should be considered in the differential diagnosis of inguinal masses in adult females. The successful laparoscopic management demonstrates the effectiveness of this surgical approach. Further systematic review is warranted to refine diagnostic and treatment protocols for this uncommon but clinically significant condition [14].
Conflict of interest statement
None declared.
Funding
None declared.
References
Fikatas P, Megas IF, Mantouvalou K, et al.



