-
PDF
- Split View
-
Views
-
Cite
Cite
Arunan Mahendravarman, Dulani Goonawardhana, Philip Le Page, Surgical resection of Killian-Jamieson esophageal diverticulum, Journal of Surgical Case Reports, Volume 2025, Issue 9, September 2025, rjaf724, https://doi.org/10.1093/jscr/rjaf724
Close - Share Icon Share
Abstract
Killian-Jamieson diverticulum (KJD) is an exceptionally rare esophageal diverticulum arising below the cricopharyngeal muscle, distinguished from the more common Zenker’s diverticulum. We present a 57-year-old male with dysphagia, regurgitation of undigested food, and globus sensation. Fluoroscopic swallow study demonstrated a left-sided KJD. Given his significant symptoms and the close proximity to the recurrent laryngeal nerve, an open transcervical diverticulectomy was performed with careful recurrent laryngeal nerve preservation. Post-operative recovery was uneventful with no residual diverticulum or leak on imaging. This case highlights the importance of distinguishing KJD from Zenker’s diverticulum, as surgical approaches differ due to anatomical considerations. Open resection remains the preferred option for symptomatic KJD to ensure safe excision and nerve preservation.
Introduction
Esophageal diverticulum is a relatively rare disorder of the esophagus in which there is an outpouching of the esophageal mucosa. These diverticula are characterized by their anatomical location. First described in 1983, a Killian-Jamieson diverticulum (KJD) is the rarest, with an incidence of 0.025% in the general population [1]. A KJD arises distal to the cricopharyngeal muscle, lateral from the Killian-Jamieson space, distinguishing it from the more commonly known Zenker's diverticulum (ZD), which arises above the cricopharyngeal muscle and extends posteriorly. Both can be asymptomatic, or patients can present most commonly with dysphagia or regurgitation.
Case
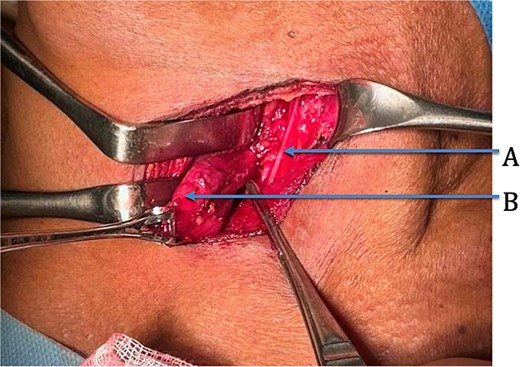
We present the case of a 57-year-old male patient who presented with dysphagia, regurgitation of undigested food, alongside a globus sensation. He had no significant medical history. He underwent a fluoroscopic swallow study, which revealed an anterolateral pharyngeal diverticulum consistent with a KJD with a neck of 5 mm and a length of 25 mm (Fig. 1). Given his symptoms, operative management was undertaken in which an incision was made along the medial border of the sternocleidomastoid. The platysma was divided, and dissection performed down to the level of the thyroid membrane with preservation of strap muscles. The left recurrent laryngeal nerve (RLN) was identified and preserved (Fig. 2). The esophageal diverticulum and sac were isolated from surrounding structures, and the neck was ligated using a 2/0 Vicryl prior to being excised. The ligation site was oversewn with 3/0 Vicryl. A drain was left, and the incision was closed in layers. Post-operatively, the patient underwent fluoroscopic swallow study, which did not show a leak or residual diverticulum, and after removal of the drain, the patient was discharged home day 1 postoperatively (Fig. 3).

Coronal view of fluoroscopic swallow showing Killian-Jamieson esophageal diverticulum labeled A.

Coronal view of postoperative fluoroscopic swallow study demonstrating no evidence of remnant diverticulum or leak.
Discussion
Symptomatic KJD usually presents with dysphagia secondary to solids, and due to its lower location, aspiration is not often seen. Asymptomatic patients often have an esophageal diverticulum incidentally noted on cervical ultrasound, with reports frequently describing the diverticulum as a possible thyroid nodule [2]. Clinically, it is important to understand that management for KJD and ZD differ due to their location. Management depends on severity of symptoms and size and can be open or endoscopic.
Previous reports have highlighted the benefit of endoscopic treatments of ZD [3–5], as a minimally invasive approach. An endoscopic approach is, however, less favored in KJD due to its proximity to the RLN [6, 7] which enters the pharynx through the Killian-Jamieson space. As seen in Fig. 2, the RLN is visualized coursing close to the neck of the KJD. Open approach enables direct visualization of the nerve when compared to an endoscopic approach. Cricopharyngeal myotomy (CPM) is often recommended in the management of ZD, given cricopharyngeal muscle dysfunction playing a major role in its etiology. Due to its location below the cricopharyngeus, CPM is not considered to be central to definitive management of KJD [8].
Overall, it is important to delineate the difference between ZD and KJD to determine management approaches. Open transcervical diverticulectomy for symptomatic KJD provides patients with definitive management and minimal morbidity.
Conflict of interest statement
None declared.
Funding
None declared.



