-
PDF
- Split View
-
Views
-
Cite
Cite
Liam Strabac, Kathryn McLeod, Rick Catterwell, Richard Grills, A TURP without a foot pedal—making do in a resource poor setting, Journal of Surgical Case Reports, Volume 2025, Issue 9, September 2025, rjaf703, https://doi.org/10.1093/jscr/rjaf703
Close - Share Icon Share
Abstract
Delivering surgical services in low- and middle-income countries often requires adaptability and ingenuity due to resource limitations. This case report describes how a visiting surgical team in a Pacific Island nation overcame the absence of a diathermy foot pedal during a transurethral resection of the prostate by collaborating with both on-site and remote biomedical engineers. The team modified a handheld pencil diathermy to mimic foot pedal functionality. The procedure was successfully completed without complications. This case highlights the challenges faced by visiting teams in low- and middle-income countries and the importance of collaboration and innovation in overcoming equipment shortages.
Introduction
The Royal Australasian College of Surgeons (RACS) through the Global Health Programme provides outreach services to Pacific Island nations [1]. Yearly visits enable locals to access treatment for various conditions including benign prostatic hyperplasia (BPH). Transurethral resection of the prostate (TURP) is the gold-standard treatment for BPH and relies on electrosurgical equipment readily available in high-income countries (HICs). In resource-limited settings, challenges arise when standard equipment is nonfunctional or unavailable. We present a case where a planned TURP procedure was interrupted due to the absence of a diathermy foot pedal, requiring an improvised solution to proceed.
Case report
A patient with BPH was scheduled for TURP in a Pacific Island nation. The operation was to be completed by the visiting surgical team from Australia. After the patient was brought to the operating theatre and received general anaesthesia, a standard cystoscopy was performed. As the visiting team prepared to proceed with the TURP, and the electrosurgical unit (ESU) settings had been set, a foot pedal to activate the diathermy current was requested. The Pacific Island home team revealed that a foot pedal was unavailable and could not be sourced for several days. Faced with this delay, the operation was abandoned, and the patient was returned to the ward whilst the team explored alternative solutions.
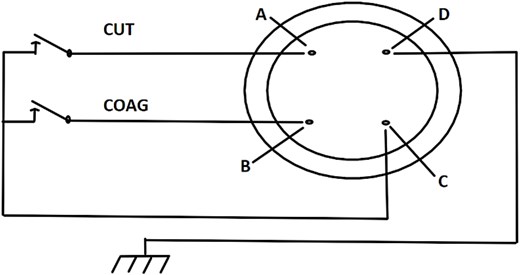
Due to logistical constraints, the surgical team could not wait for the foot pedal to arrive. It was proposed, with the assistance of an on-site biomedical engineer, to modify a handheld pencil diathermy unit to serve as a proxy foot pedal. To ensure the feasibility and safety of this solution, the team contacted the biomedical engineering department in an Australian hospital for remote assistance. The Australia-based engineers provided wiring diagrams (Fig. 1), troubleshooting advice and guidance, liaising with the on-site engineer to rewire the diathermy unit.
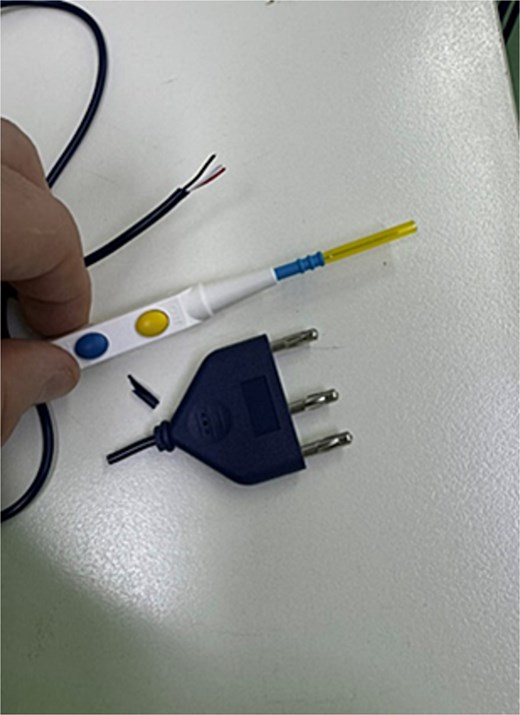
The cables of the diathermy were separated (Fig. 2) and connected to the corresponding pins on the monopolar footswitch socket of the ESU (Fig. 3). A multimeter was utilized to ensure safety and compatibility of the diathermy with the ESU. By interfacing the pencil diathermy with the foot pedal input source on the ESU, the team used the pencil’s manual on/off function to mimic that of the foot pedal.

Pencil diathermy cables inserted into respective pins of monopolar footswitch socket of ESU.
The diathermy was then held by the surgical assistant (Fig. 4), who controlled its activation under the surgeon’s command, whilst the surgeon completed the TURP using the working element in the usual fashion. This workaround enabled the team to successfully proceed with the operation on this patient the following day despite the lack of a foot pedal. No intraoperative or post operative complications occurred, and the patient was discharged on the 2nd post operative day.

The lead surgeon operates whilst the surgical assistant controls the handheld diathermy.
Discussion
This case highlights the practical challenges visiting teams must navigate when providing care in low- and middle-income countries (LMICs). The absence of a critical piece of equipment necessitated an improvised solution to proceed with the TURP. To ensure safety, a multimeter was used to confirm the modified circuit remained inactive at rest and only allowed current to flow when the button was pressed, mimicking foot pedal functionality. It also confirmed the absence of any stray current or electrical leakage which could otherwise pose a risk of burns or equipment malfunction. Bypassing the foot pedal without conducting safety checks could result in continuous diathermy activation or electrical injury. Any such replication of this improvisation should not be done without engineering oversight.
This example illustrates the adaptability required of visiting teams and the systemic challenges faced in LMICs, including the absence of standard equipment, reliance on outdated or inadequately maintained devices, and the need to repurpose materials for non-standard uses [2–4]. In such situations, having access to remote contacts can greatly enhance problem-solving capacity. In this case, colleagues in Australia provided wiring diagrams and technical guidance via text messages, helping the team safely modify equipment to proceed with the procedure. Establishing networks of remote contacts allows visiting teams to leverage external expertise in real-time, addressing complex problems whilst maintaining patient safety.
In LMICs, urologists report challenges with facilities, sufficiently trained staff, and materials. These challenges are cited more frequently by visiting urologists, possibly reflecting their familiarity with the resource-rich settings of HICs [5]. It is common for visiting urologists to bring materials with them on outreach visits, but they are often limited by the costs of freight. Visiting teams may also be responsible for sterilizing and maintaining the equipment they bring, as local facilities often lack the capacity to do so [4].
To address chronic shortages in local facilities, LMICs rely heavily on donations. However, donation of medical equipment is fraught with challenges such as the inevitable use of expired materials and reuse of single-use materials by local surgeons [3]. Additionally, local facilities may lack the ability to maintain and repair medical devices, reducing the lifespan of donated equipment [6]. In settings where comprehensive inventories are not comprehensive, and communication is challenging, visiting urologists may not have an accurate representation of equipment and materials until it is needed intra-operatively [7]. Therefore, utilizing local items in procedures requires careful consideration. For example, whilst using bladder irrigation fluid that expired 1 month prior may be considered safe, using irrigation fluid that expired 5 years ago could pose significant risks. In such cases, visiting teams must balance safety with the practical realities of delivering much needed surgical services and the consequences of not doing so.
The combination of high patient demand, time constraints of outreach visits, and the limited availability of functioning medical equipment in LMICs requires surgeons to be highly adaptable. Chronic shortages of essential equipment often lead to the non-standard use of various materials in LMICs. Examples of such ingenuity include the reported use of Foley catheters as makeshift chest drains and gastrostomy tubes, and the inner tubing of bicycle tyres as tourniquets due to scarcity of supplies [2]. Alternative surgical techniques have also been employed, such as the use of room air for mechanical insufflation in laparoscopic cholecystectomies [8]. These examples represent just a fraction of the ingenuity shown in LMICs and likely do not capture the full extent of improvisation as most innovations may go undocumented due to the challenges of publishing in these settings [9]. The ability to repurpose materials and adapt to chronic supply shortages underlines the resourcefulness required of both visiting and local surgeons in LMICs. Whilst improvised solutions are often necessary in LMICs, they also highlight the need to develop sustainable methods to strengthen medical supply chains and local infrastructure.
Acknowledgements
The authors wish to thank the biomedical engineers for their remote support and technical guidance. We also acknowledge the dedicated staff in Tuvalu for their collaboration and support during the outreach visit.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This work was not supported by any funding sources.



