-
PDF
- Split View
-
Views
-
Cite
Cite
Mar Cotter, Ciara Walsh, Dhruv Kapoor, Chloe Spillane, Jemima Dorairaj, Burning love: digital escharotomy in the management of an electrothermal wedding band burn from a lawnmower battery. A case report, Journal of Surgical Case Reports, Volume 2025, Issue 9, September 2025, rjaf660, https://doi.org/10.1093/jscr/rjaf660
Close - Share Icon Share
Abstract
Reporting of electrothermal ring burns in the literature is infrequent and comprise of a minimal amount of burn consults with no existing standardized approach to treatment and management. They are, however, a potentially serious burn as they have a propensity to be circumferential given the circular nature of rings, increasing the risk of compartment syndrome which may result in irreversible neurovascular damage and potential digit amputation if not treated in a timely manner, despite the very small total body surface area of the burn. This case report has demonstrated the success of digital escharotomy in the management of electro thermal ring injuries.
Introduction
Injuries from electrothermal ring burns are based on both the electrical current and the alloy or metal [1]. High-voltage injuries occur more commonly in occupation-related accidents especially those with the automotive industry. Thermo-electrical burns from gold occur when an electrical current passes through the conductive metal, generating intense heat, causing severe burns upon skin contact. Gold’s excellent conductivity and low resistance allow it to rapidly reach high temperatures when electrified [2]. Such burns can result in neurovascular injury and amputation at worst. Management depends on the severity of the burn and includes conservative management, amputation [3], and escharotomy [4].
Case report
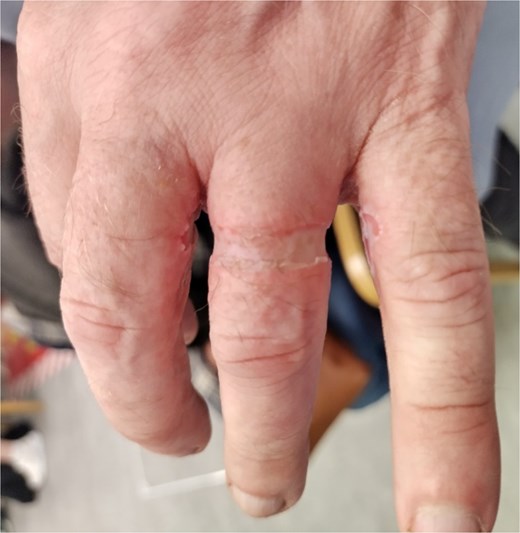
A 62 year old male maintenance operator with no significant medical or surgical history sustained a workplace related, electrothermal deep dermal circumferential burn to his left ring finger on his non dominant hand. Whilst changing a 12-volt lawnmower battery, his wedding band inadvertently came in contact with the negative electrode. A spanner in his right hand, simultaneously came in to contact with the positive electrode, thus short circuiting. The resultant electrothermal injury measured 18 mm in diameter, 4 mm wide, and 1.5 mm thick, corresponding to his wedding band. Fifteen minutes postinjury, he attended his nearby local injuries unit. He was alert, oriented to person, place, and time and haemodynamically stable. ECG demonstrated normal sinus rhythm. Ninety minutes postinjury, the area was white and non-blanching with superficial burns on the radial side of the little finger and ulnar side of the middle finger (Figs 1–3). On examination, the finger was neurovascularly intact, capillary refill time <2 s, and the patient had full range of active and passive motion on both extension and flexion of the metacarpal phalangeal, proximal interphalangeal and distal interphalangeal joints. This was repeated by the same clinician prior to transfer and remained unchanged. The patient was transferred to a level one trauma centre under the care of plastic and reconstructive surgery. Examination was consistent with a deep dermal burn, of <0.2% total body surface area as per Lund and Browder charting as above. Four hours postinjury capillary refill time was now >2 s. Sensation was reduced and swelling increased with a marginal reduction of both flexion and extension at both the proximal interphalangeal and distal interphalangeal joints (Figs 4 and 5). Given the circumferential nature of the burn, increasing swelling and observed circulatory and sensory changes, surgical intervention via radial escharotomy was undertaken as opposed to a conservative ‘watch and wait’ approach. A 1.5 cm incision (Fig. 6) from normal to normal tissue, traversing the burn was made midway between the mid-axial line and the extensor tendon so as to minimize risk to the neurovascular bundle as per emergency management of severe burns [5]. A radial border incision only, is to minimize risk to the ‘working border’. Unlike limb or chest escharotomies, digital escharotomies do not require both sides to be released. This was completed under local anaesthesia using 5 ml of both plain 2% lidocaine and 0.25% Bupivacaine via ring block. Skin tension was immediately released on incision, as seen in Fig. 6 and left to heal by secondary intention and it was clinically evident that there would be undue tension on the tissue if closed primarily. Dressing was with mepitel, gauze, and cling and support with a Bradford sling. The patient was discharged home well on day 3 postop. Swelling had reduced, the finger was neurovascularly intact, and flexion and extension was restored (Figs 7 and 8).







The patient returned for weekly review. Hand physiotherapy to achieve both a baseline range of motion and hand strength was initiated after 1 week. Scar management via massage therapy was initiated at week 4. At week 12, there was excellent healing as per patient healing outcome, without any indication of contracture, neurovascular deficits, limitations in movement, or significant scar formation (Figs 9 and 10).


Discussion
Electrothermal burn injuries from rings represent a small proportion of presentations to burn injuries units [6]. The mechanism of injury in this case involved the conversion of an electrical current from a 12-volt automotive battery and the resistance of the body tissues through which it passed, the left ring finger, into the thermal energy resulting in tissue damage. Bone, tendon, muscle, fat, and skin are high-resistance tissues and when exposed to high-voltage electricity, they will heat up and coagulate. The thermal conductivity of a metal, in this case, a gold wedding band also determines the extent of the injury. Metals with higher thermal conductivity become hotter in a shorter amount of time for a given amount of energy and cause greater tissue damage [7].
To understand the zones of injury, it is necessary to discuss Jackson’s thermal wound theory [8]. Accordingly, there are three zones of burn injury:
Zone of coagulation: Is the area of tissue that sustains the most damage from the heat source, at the time of injury. Here, tissue loss is irreversible due to coagulation of the constituent proteins.
Zone of stasis: This zone surrounds the zone of coagulation. It is characterized by inflammation and is poorly perfused.
Zone of hyperaemia: This is the outermost zone which maintains its microvascular circulation.
Each zone is dynamic and time can transform from what was initially viable tissue to non-viable tissue which underpins the rational of a burn being left to declare itself prior to surgical intervention unless other circumstances prove urgent [9]. In this case, evolving circulatory compromise expedited surgical intervention via escharotomy.
Management of thermoelectrical ring burns as reported in the literature is variable. Conservative management, primary closure, escharotomy, full thickness skin grafting, allogeneic grafting, adipofascial turnover flaps and when these modalities have failed, amputation have all been employed [10, 11]. The multiple treatment options highlight two key points. First, that management is very much anecdotal, based on clinical expertise and experience on a case to case basis, and secondly that a standardized approach is required to ensure optimal patient outcome [12]. This case report has demonstrated the success of digital escharotomy in the management of this electrothermal injury, but it also notes that management must be tailored to each case in conjunction with the clinical acumen of the operating surgeon.
Conflict of interest statement
None declared.
Funding
No financial support was sought or received for this research.
References
Emergency Management of Severe Burns. https://www.britishburnassociation.org.



