-
PDF
- Split View
-
Views
-
Cite
Cite
Salman Abdullah Aljubori, Rouz Faisal Abu Sulami, Abdullah Khalid Aljohani, Maram Mohammed Zahid, Sally Osama, Hiatal hernia complicated by gastric volvulus: case report, Journal of Surgical Case Reports, Volume 2025, Issue 9, September 2025, rjaf648, https://doi.org/10.1093/jscr/rjaf648
Close - Share Icon Share
Abstract
Gastric volvulus is a rare and potentially life-threatening complication of large hiatal hernias. It is defined as the abnormal rotation of the stomach by >180° around one of its axes, leading to closed-loop obstruction and risks of ischemia and perforation. We present a case of an 84-year-old female presented with severe epigastric pain associated with coffee ground vomiting. Esophagogastroduodenoscopy and computed tomography scan confirmed a large hiatal hernia complicated by gastric volvulus. Surgical intervention was done with a tension-free gastropexy following a partial reduction of the hiatal hernia. Postoperative recovery was closely monitored in the intensive care unit, and the patient gradually improved and was discharged home after 17 days. This report highlights the importance of considering gastric volvulus in the differential diagnosis of upper abdominal pain and vomiting, particularly when associated with hiatal hernia in elderly patients.
Introduction
Gastric volvulus is a rare, life-threatening complication of a large hiatal hernia, typically characterized by Borchardt’s triad, which includes intense epigastric pain, retching, and difficulty with nasogastric tube insertion. It occurs when the stomach or part of it rotates by >180° around one of its axes, leading to a closed-loop obstruction. Gastric volvulus is associated with high morbidity and mortality rates, 30%–50%, primarily due to gastric ischemia, perforation, and necrosis, highlighting the importance of early diagnosis and prompt surgical management [1]. This case report emphasizes the importance of maintaining a high index of suspicion for gastric volvulus in the differential diagnosis of abdominal pain associated with hiatal hernia in elderly patients.
Case report
An 84-year-old female patient with no significant medical or surgical history. She was presented to the emergency department complaining of severe epigastric pain associated with two episodes of coffee ground vomiting, which had been ongoing for 1 day before admission. She had experienced a similar episode of coffee ground vomiting 3 months prior, which had improved with antacid therapy. Furthermore, she reported chronic epigastric pain, gastric reflux, early satiety, and exertional dyspnea with minimal physical activity.
Upon admission, the patient appeared ill, and vital signs were as follows: temperature 37°C, blood pressure 180/80 mmHg, heart rate 82 bpm, oxygen saturation 92%, and random blood sugar 149 mg/dl. On abdominal examination, tenderness was noted in the epigastric and left hypochondriac regions. Chest examination revealed equal bilateral air entry. Venous blood gas showed uncompensated respiratory acidosis with pH: 7.28, PaCO₂: 59 mmHg, and HCO₃−: 24 mmol/L. Routine laboratory investigations were within normal limits. An abdominal ultrasound was performed, but the findings were inconclusive. An abdominal computed tomography (CT) scan demonstrated a large hiatal hernia, with a dilated gastric fundus and pylorus herniating through the hiatus into the thoracic cavity. With internal hyperdense content, representing food particles or hemorrhagic components. It was causing a mass effect on the mediastinal structures. Gastric volvulus's suggestive finding was the marked gastric distention with two distinct areas of distention, consistent with the torsion of gastric volvulus (Fig. 1). Esophagogastroduodenoscopy (EGD) revealed a twisted stomach along its central axis, filled with food and coffee ground content, and the pylorus could not be visualized, suggesting gastric volvulus.
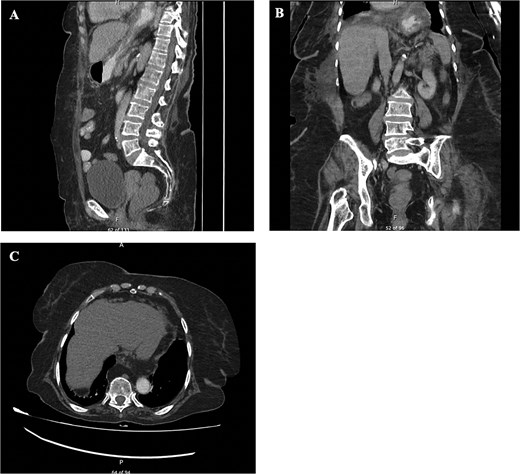
CT finding. (A) CT scan of abdomen, sagittal view. (B) CT scan of abdomen, coronal view. (C) CT scan of abdomen, axial view. Showing a large hiatal hernia with dilated gastric fundus and pylorus. With internal hyperdense content, representing food particles or hemorrhagic components. It is causing a mass effect on the mediastinal structures. Gastric volvulus's suggestive finding is the marked gastric distention with two distinct areas of distention, consistent with the torsion of gastric volvulus.
Inserting a nasogastric tube for gastric decompression was difficult, requiring several attempts. The patient underwent a laparotomy due to the high risk of gastric ischemia and perforation. During laparotomy, the stomach was found to be partially sliding into the thoracic cavity. The orientation of the stomach appeared normal, with signs of gastric ischemia and inflammatory edema, indicating a resolving gastric volvulus. A trial of blunt dissection was performed to reduce the proximal part of the stomach from the thoracic cavity, resulting in partial reduction of the herniating stomach, as a complete reduction was not possible due to esophageal shortening and retraction. A tension-free gastropexy was performed, securing the stomach to the anterior abdominal wall.
Postoperatively, the patient was monitored closely in the intensive care unit and managed with intravenous fluids for electrolyte disturbance and oxygen therapy via nasal cannula for low oxygen saturation associated with bilateral mild pleural effusion. The patient gradually improved and was discharged home after 17 days.
Discussion
Gastric volvulus is a rare and potentially life-threatening condition characterized by the abnormal rotation of the stomach around one of its axes, leading to closed-loop obstruction and risks of strangulation, ischemia, necrosis, and perforation. This condition predominantly affects the elderly, with peak incidence observed around the age of 50 [1]. About 30% of gastric volvulus cases are primary idiopathic; however, most of the cases are secondary to hiatal hernia, traumatic diaphragmatic defects, diaphragmatic eventration, and phrenic nerve paralysis [2]. The association between hiatal hernia and gastric volvulus is well-established [1].
Gastric volvulus is classified into four types based on the axis of rotation. Type 1, organoaxial volvulus, involves the rotation of the stomach around the pylorus-cardia axis and accounts for ~60% of cases. Type 2, mesenteroaxial volvulus, involves the rotation around an axis bisecting the greater and lesser curvatures. Type 3 is a combination of organoaxial and mesenteroaxial rotation, comprising 2% of cases. While Type 4 remains unclassified, it constitutes 10% of cases [3].
Gastric volvulus typically presents with severe epigastric pain, unproductive retching, and difficulty inserting a nasogastric tube, known as Borchardt's triad, which is present in 70% of cases [1]. Additionally, gastric volvulus can present with hematemesis due to gastric mucosal tear or ischemia [4]. Chronic presentation of volvulus includes dysphagia, postprandial discomfort, vomiting, and dyspnea [5]. In our case, the patient demonstrated Borchardt's triad with severe epigastric pain, gastric reflux with retching, and difficult insertion of the nasogastric tube requiring several attempts, along with two episodes of coffee-ground vomiting.
Diagnosis of gastric volvulus depends on the clinical presentation along with the imaging findings [6]. Abdominal CT scan can reveal evidence of anatomical defect, stomach wall pneumatosis, and perforation [7]. EGD is a diagnostic and therapeutic modality. Acute gastric volvulus endoscopic findings include mucosal congestion and inability of the scope to pass through the pylorus. Endoscopic reduction of a chronic gastric volvulus has been reported in the literature, with caution taken to prevent causing perforation [8].
Acute management of gastric volvulus consists of resuscitation and nasogastric tube placement [1]. Surgical approach comprises the mainstay of the treatment [2]. The surgical intervention includes stomach decompression, volvulus reduction, correction of the intra-abdominal factors predisposing to volvulus, including hiatal hernia, and finally, gastropexy to prevent recurrent volvulus. In complicated cases with gangrene or perforation, partial or total gastrectomy may be necessary [9]. Our patient underwent laparotomy, which revealed gastric ischemia and inflammatory edema, indicating a resolving volvulus. A trial of blunt dissection was performed to reduce the hiatal hernia, then gastropexy was performed to secure the stomach to the anterior abdominal wall, preventing recurrence. This case highlights the importance of considering gastric volvulus in the differential diagnosis of upper abdominal pain and vomiting when associated with hiatal hernia in elderly patients.
Conflict of interest statement
None of the authors has any conflicts of interest to disclose concerning this article.
Funding
None declared.



