-
PDF
- Split View
-
Views
-
Cite
Cite
Yassine El Bouazizi, Amine El Bouazizi, Sabrillah Echiguer, Mohammed R El Hassouni, Amina Houmada, Zakaria El Mouatassim, Oumaima Lahnaoui, Mohammed A Majbar, Amine Souadka, Amine Benkabbou, Laparoscopic hepatic resection for metastatic recurrence on hepatectomy margin: a novel traction technique using previously placed locking clips, Journal of Surgical Case Reports, Volume 2025, Issue 8, August 2025, rjaf623, https://doi.org/10.1093/jscr/rjaf623
Close - Share Icon Share
Abstract
Recurrent hepatic metastases at the resection margin following laparoscopic hepatectomy present technical challenges due to adhesions and altered anatomy. We describe an innovative traction technique using locking clips to facilitate safe re-resection. A 65-year-old patient with colorectal liver metastasis in segment 6 underwent laparoscopic hepatectomy. Three years post-operatively, imaging revealed recurrence at the hepatectomy margin. We describe a novel technique utilizing previously placed locking clips from the initial surgery as traction elements to provide optimal exposure during laparoscopic re-resection. The technique involves repurposing locking clips that were placed during the initial hepatectomy for hemostasis, using them as traction elements to create controlled manipulation of liver segments, allowing safe dissection and optimal visualization of the recurrent lesion, particularly valuable in peripheral hepatectomies. This innovative technique of repurposing previously placed locking clips as traction elements represents a valuable addition to the laparoscopic hepatobiliary surgeon’s armamentarium for managing recurrent hepatic metastases.
Introduction
Laparoscopic hepatectomy has become the gold standard for selected hepatic metastases, offering reduced morbidity and faster recovery compared to open surgery [1, 2]. However, local recurrence at the resection margin remains a significant challenge, occurring in 10%–15% of cases [3]. Re-resection of recurrent hepatic metastases presents unique technical difficulties due to adhesions, altered anatomy, and the need for precise identification of the recurrence site [4].
Traditional approaches to hepatic re-resection often require conversion to open surgery due to visualization challenges and difficulty in achieving adequate traction [5]. We present an innovative laparoscopic technique utilizing previously placed locking clips from the initial hepatectomy as traction elements to facilitate safe and effective re-resection of recurrent hepatic metastases at the hepatectomy margin.
Case presentation
A 65-year-old patient with a history of colorectal cancer presented with a solitary hepatic metastasis in segment 6. Initial treatment consisted of laparoscopic wedge resection with negative margins (R0 resection). During the initial procedure, several locking clips were placed for hemostasis along the resection margin and adjacent hepatic tissue. Histopathology confirmed complete excision of a 3.5 cm moderately differentiated adenocarcinoma metastasis.
Three post-operatively, routine surveillance imaging (computed tomography and magnetic resonance imaging) revealed a 2.2 cm recurrent lesion at the previous hepatectomy margin in segment 6. The patient was asymptomatic with normal liver function tests (aspartate aminotransferase: 28 U/L, alanine aminotransferase: 32 U/L, bilirubin: 12 μmol/L). Multidisciplinary team discussion concluded that laparoscopic re-resection was feasible and appropriate.
Surgical technique
Preoperative planning
High-resolution computed tomography with arterial and portal venous phases
MRI with hepatobiliary contrast for precise localization
Virtual 3D reconstruction to assess relationship to vascular structures
Preoperative marking of the recurrence site using ultrasound guidance
Operative setup
Patient positioned supine with left side elevated 30°
Five-port laparoscopic approach with CO2 insufflation at 12 mmHg
0° laparoscope for optimal visualization
Harmonic scalpel and bipolar electrocautery available
Pringle maneuver capability if required.
Novel traction technique using previously placed clips
Step 1: Assessment and identification of existing clips.
Initial laparoscopic exploration revealed dense adhesions at the previous resection site with fibrous tissue surrounding the recurrent lesion. Careful adhesiolysis was performed to identify anatomical landmarks and locate the locking clips placed during the initial hepatectomy (Fig. 1).
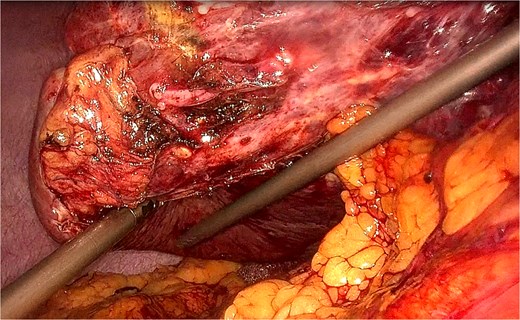
Laparoscopic view showing adhesiolysis and mobilization of the right liver lobe with identification of the locking clip on the margin of the previous S6 hepatectomy. Dense adhesions are visible at the resection site, requiring careful dissection to locate the previously placed hemostatic clip.
Step 2: Clip identification and assessment
Key Innovation: The locking clips placed during the initial surgery for hemostasis were identified and assessed for their potential use as traction elements.
The clips had maintained their position and integrity, providing ideal anchor points for traction (Fig. 2).
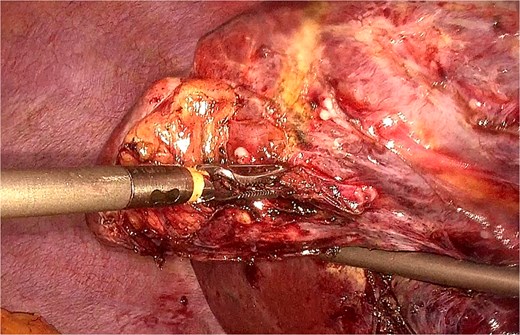
Close-up laparoscopic view demonstrating precise identification of the locking clip that will serve as the traction element. The clip maintains its structural integrity and positioning 3 years after the initial hepatectomy, providing an ideal anchor point for liver manipulation.
Step 3: Repurposing clips for traction
Using laparoscopic graspers, the existing locking clips were engaged and repurposed as traction elements. This innovative approach offered several advantages:
Predetermined positioning: Clips were already optimally placed from the initial surgery
Multidirectional traction: Clips allowed 360° manipulation of liver segments (Fig. 3)
Stable grip: Locking mechanism provided consistent traction force
Tissue preservation: No additional trauma from new clip placement
Optimal exposure: Enhanced visualization of critical structures around the recurrence (Fig. 4)
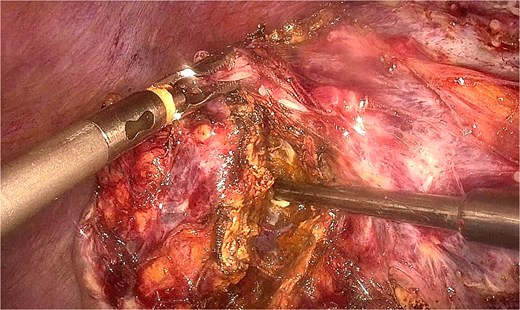
Demonstration of multidirectional liver manipulation using the repurposed locking clip as a traction element. The clip allows 360° manipulation of the liver segment, providing optimal exposure of the recurrent lesion and surrounding structures during dissection.

Laparoscopic view showing how the clip-assisted traction optimally exposes the vascular structures requiring ligation during the re-resection. The enhanced visualization allows for safe identification and control of hepatic vessels while maintaining adequate surgical margins around the recurrent metastasis.
Step 4: Resection
With adequate traction and exposure achieved, the recurrent lesion was carefully dissected. Intraoperative ultrasound confirmed complete visualization of the tumor and its relationship to hepatic vessels. A 1 cm margin was achieved circumferentially.
Step 5: Hemostasis and closure
Following resection, hemostasis was achieved using bipolar electrocautery and hemostatic agents. The repurposed clips remained in place as they continued to provide hemostatic benefit. The resection bed was inspected for bleeding. A Jackson-Pratt drain was placed.
Discussion
Technical advantages
The described technique of repurposing previously placed locking clips offers several advantages over conventional methods:
(1) Optimal pre-positioning: The clips were already ideally positioned from the initial surgery, eliminating the need for additional clip placement and reducing operative time [6].
(2) Enhanced visualization: The ability to manipulate liver segments using existing clips provides optimal exposure of the surgical field, particularly crucial in peripheral hepatectomies where access can be challenging [7].
(3) Reduced tissue trauma: Unlike placing new clips or using other traction methods, repurposing existing clips avoids additional tissue manipulation and potential complications [8].
(4) Cost-effectiveness: Utilizing existing clips reduces the need for additional surgical materials and operative time.
(5) Anatomical familiarity: The clips serve as anatomical landmarks, helping orient the surgeon to the previous surgical field and critical structures.
Clinical implications
Recurrent hepatic metastases present significant challenges, with traditional approaches often requiring conversion to open surgery. Our technique demonstrates that complex laparoscopic re-resections can be performed safely by repurposing surgical materials from the initial procedure, representing a paradigm shift in resource utilization [9].
The oncological outcomes in our case are encouraging, with R0 resection achieved and no recurrence at 12 months follow-up. This aligns with recent literature suggesting that laparoscopic re-resection can achieve similar oncological outcomes to open surgery when appropriate techniques are employed [10].
Conclusion
We present a novel laparoscopic technique utilizing previously placed locking clips from the initial hepatectomy as traction elements during hepatic re-resection of recurrent metastases. This approach offers optimal pre-positioning, enhanced visualization, and reduced tissue trauma while being cost-effective and utilizing existing surgical materials. The technique represents a valuable addition to the minimally invasive hepatobiliary surgeon’s armamentarium and may help reduce the need for conversion to open surgery in selected cases.
Conflict of interest statement
The authors declare no conflicts of interest.
Funding
No funding was received for this study.
Ethical approval
This case report was conducted in accordance with institutional guidelines and patient consent was obtained.



