-
PDF
- Split View
-
Views
-
Cite
Cite
Ali Adwal, Ahmed M Suleiman, Anmar M Ahmed, Mahmood Adwal, Muntadher Y H Al Gehadi, Sajjad Ghanim Al-Badri, Rhinophyma treated by skin graft: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 8, August 2025, rjaf248, https://doi.org/10.1093/jscr/rjaf248
Close - Share Icon Share
Abstract
Rhinophyma, a late-stage complication of rosacea, causes progressive nasal deformity characterized by hypertrophy and fibrosis of sebaceous glands. Surgical excision is the primary treatment, and various techniques are available. This case report highlights a 70-year-old male treated with full-thickness excision and skin grafting, demonstrating successful outcomes. The review underscores the importance of personalized surgical approaches to achieve optimal results in rhinophyma management.
Introduction
Rhinophyma is a condition causing the development of a large, bulbous nose associated with granulomatous infiltration, commonly due to untreated rosacea [1].
The condition is most common in older white males [2]. Colloquial terms for the rhinophyma include “whiskey nose”, “gin blossom”, “toros nose”, and “potato nose”. Rhinophyma is characterized by hypertrophy of nasal skin, with hyperplasia and fibrosis of the sebaceous glands and connective tissue. The nasal tip and alae are preferentially affected by the hypertrophy, and the lower portion of the nose is predominantly affected. The underlying bony structure is not affected [2].
The exact cause of rhinophyma is unknown; it is believed to be multifactorial in origin with a principal etiology of unregulated superficial vasodilation. Surgical intervention remains the only effective treatment, with various techniques proposed; however, no single approach is considered the definitive gold standard [1].
Case presentation
A 70-year-old man presented to the outpatient dermatology clinic with a progressively enlarging, bulbous nasal deformity over the past 10 years. His medical history was significant for acne rosacea, while his surgical history was unremarkable.
On physical examination, there was notable soft tissue hypertrophy of the nose, irregular in shape but without ulceration or bleeding. The lesion was confined to the nasal region (Fig. 1). Based on clinical findings, a diagnosis of rhinophyma was established.
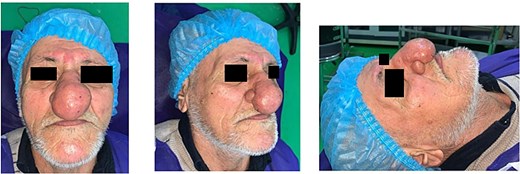
Preoperative view; showing a 70-year-old male with nasal soft tissue swelling, irregular in shape, no ulceration, no bleeding, and lesion confined to the nose.
The surgical intervention involved the complete excision of the nasal tumor while preserving the underlying cartilage, perichondrium, and periosteum (Fig. 2). Hemostasis was achieved using peritumoral injections of saline and adrenaline. During the same procedure, the resulting skin defect was covered, ensuring adequate protection of the exposed cartilage and perichondrium.
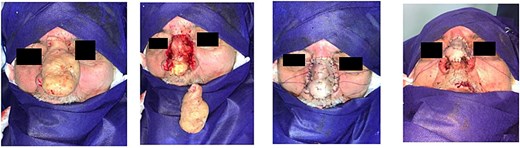
Postoperatively, a tie-over dressing was applied and maintained for 5 days to ensure graft adherence. The patient received prophylactic mupirocin ointment daily, along with wound care instructions. The stitches were removed 7 days after the surgery. The patient's recovery was uneventful, and he was discharged 10 days after the surgery with satisfactory healing.
Postoperative images (Fig. 3) were taken a few months after surgery. Long-term follow-up at 2 years (Fig. 4) demonstrated stable results with no recurrence, secondary infection, or significant scarring.


Discussion
Rhinophyma is a benign skin condition marked by tumorous enlargement, resulting in a bulbous, erythematous nasal appearance. It is recognized as a feature of advanced-stage rosacea. The cause of rhinophyma remains unknown; however, it is thought to have a multifactorial origin, with dysregulated superficial vasodilation as a primary factor. This vascular leakage results in chronic dermal interstitial edema, triggering local inflammation, fibrosis, and hyperplasia of the dermis and sebaceous glands. Over time, these changes contribute to the characteristic bright red to purplish telangiectasias and the irregular, lobulated thickening of the nasal skin [1].
While rosacea is a common condition found in women, rhinophyma is a rare disease, as reported in most studies on this disease. We have observed 12 cases over 12 years in our clinic. This disease affects older people with a mean age of 71 years in our series, while the youngest patient was 53 years old. This age factor has been reported in several publications [3, 4], with a mean age of 49 years in the largest published series [2]. Rhinophyma has a male predominance, as our series comprised nine men and three women. This male predominance has been reported by several authors [3, 4]. Rhinophyma is more often observed in Caucasians, as only 16.6% of our patients were non-Caucasian, like the ethnic distribution reported by Peu SC et al. [4].
Rhinophyma is primarily a clinical diagnosis, characterized by an enlarged, nodular nose. However, histopathological evaluation can be useful in ruling out conditions that resemble rhinophyma, such as angiosarcomas, squamous carcinoma, basal cell carcinoma, and sebaceous carcinoma [5].
Surgical intervention remains the only effective treatment for rhinophyma, yet no single technique is universally accepted as the gold standard. Various surgical approaches have been proposed, including tangential resection, which allows re-epithelialization from the residual deep pilosebaceous appendages [6]; full-thickness excision followed by skin grafting [7]; deep resection with autologous grafting combined with an elastin-collagen matrix [8]; a combination of dermabrasion and trichloroacetic acid application [9]; scalpel and CO₂ laser decortication [7]; and the combined use of CO₂ laser and pulsed dye laser to improve hemostasis and reduce erythema [10].
Once the decision to proceed with surgery is made, the main goal is to completely remove all diseased tissue to reduce the chance of recurrence. Superficial excision can promote spontaneous re-epithelialization, but it carries a higher risk of recurrence. On the other hand, deep excision ensures complete removal of pathological tissue but results in a defect that requires reconstruction. The choice of reconstruction method, whether a full-thickness skin graft or local flap, is influenced by factors such as the condition of the wound bed and the preferences of both the patient and surgeon. Saad and Matteucci, report a severe case of rhinophyma. Although the cartilage was not directly invaded, it became softened and distorted due to the mass effect of the condition, necessitating the use of auricular cartilage for support. A complex, three-stage forehead flap was used for reconstruction [11].
In contrast, in our case, full-thickness excision was performed followed by skin grafting for reconstruction. This case highlights the successful management of severe rhinophyma in a 70-year-old male with a history of acne rosacea. The treatment involved complete excision of the nasal tumor while preserving underlying structures, followed by skin grafting for reconstruction. It emphasizes the importance of individualized surgical approaches to ensure complete removal of diseased tissue, minimize recurrence, and optimize functional and aesthetic outcomes, particularly when dealing with complex nasal deformities due to rhinophyma.
Conclusion
Rhinophyma requires surgical intervention for effective management, with complete excision being the key to minimizing recurrence. This case demonstrates the success of full-thickness excision and skin grafting in addressing a severe deformity. Individualized treatment plans based on the patient’s condition and preferences are essential for achieving optimal aesthetic and functional outcomes.
Conflict of interest statement
The authors declare no conflict of interest in preparing this article.
Funding
This case report received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Consent
Written consent was obtained from the patient.



