-
PDF
- Split View
-
Views
-
Cite
Cite
Yassine El Bouazizi, Sabrillah Echiguer, Amine El Bouazizi, Amina Houmada, Mohammed Reda El Hassouni, Zakaria El Mouatassim, Oumaima Lahnaoui, Mohammed Anass Majbar, Amine Souadka, Amine Benkabbou, When biliary-gastric fistula mimics double gallbladder: a diagnostic challenge in acute cholecystitis, Journal of Surgical Case Reports, Volume 2025, Issue 7, July 2025, rjaf575, https://doi.org/10.1093/jscr/rjaf575
Close - Share Icon Share
Abstract
Cholecystoenteric fistulas occur in 3%–5% of patients with gallbladder disease and can create complex imaging appearances that mimic anatomical variants. Biliary-gastric fistulas are particularly rare, representing only 15% of cholecystoenteric fistulas. We report a 76-year-old male with chronic hepatic colic. Initial imaging suggested possible gallbladder malignancy with apparent double gallbladder anatomy. Magnetic resonance cholangiography revealed two distinct formations suggesting double gallbladder with single cystic duct. However, surgical exploration disclosed acute cholecystitis complicated by biliary-gastric fistula creating a pseudocystic formation that mimicked the second gallbladder. Laparoscopic approach was converted to open cholecystectomy due to severe inflammation. Histopathology confirmed benign inflammatory disease without malignancy. This case illustrates how cholecystoenteric fistulas can create imaging appearances mimicking anatomical variants such as double gallbladder. Accurate preoperative diagnosis remains challenging, emphasizing the importance of surgical exploration in complex inflammatory conditions.
Introduction
Cholecystoenteric fistulas represent a rare but significant complication of gallbladder disease, occurring in 3%–5% of patients with cholelithiasis [1]. These fistulas typically develop through a sequence of acute inflammation, necrosis, and perforation, with subsequent adherence to adjacent organs [2]. Biliary-gastric fistulas are particularly uncommon, accounting for ~15% of all cholecystoenteric fistulas, with duodenal location being more frequent [3].
The diagnostic challenge lies in the complex imaging appearances that these fistulas can create, sometimes mimicking anatomical variants such as double gallbladder [4]. Double gallbladder is a rare congenital anomaly with an incidence of 1 in 3000–4000 individuals, and its differentiation from inflammatory pseudocystic formations requires careful radiological and surgical assessment [5]. We report a case where acute cholecystitis complicated by biliary-gastric fistula created imaging findings suggestive of double gallbladder, illustrating the diagnostic complexity of this clinical scenario.
Case report
A 76-year-old male patient, WHO performance status 0, with a medical history of well-controlled hypertension presented with chronic hepatic colic without fever or biological abnormalities. The patient was a non-smoker with no history of alcohol consumption.
Initial abdominal computed tomography revealed a macro-lithiasic gallbladder with partially sclero-atrophic wall and nodular thickening of 16 mm, raising suspicion of neoplastic degeneration. Magnetic resonance cholangiography demonstrated two distinct formations in the gallbladder region, non-communicating, initially interpreted as double gallbladder with a single cystic duct (Fig. 1). The first formation appeared partially sclero-atrophic, while the second, located in the hepatogastric space, was distended with apparent lithiasic content and thickened walls. Moderate dilatation of the main and intrahepatic bile ducts was noted without identifiable lithiasic obstruction.
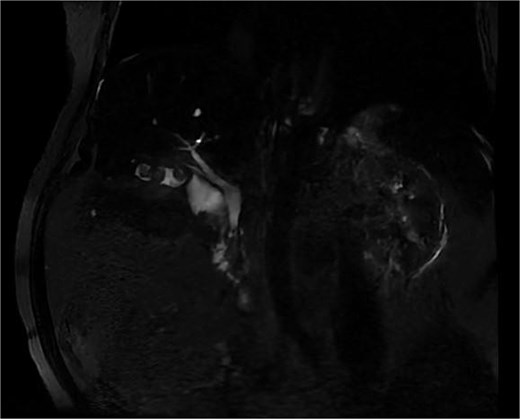
Biliary MRI showing an image mimicking a double gallbladder with a single cystic duct and an intravesicular macrolithiasis.
The imaging findings suggested a rare anatomical variant of double gallbladder complicated by inflammatory changes. Following multidisciplinary discussion, laparoscopic cholecystectomy was indicated given the suspected anatomical complexity and possible malignant transformation.
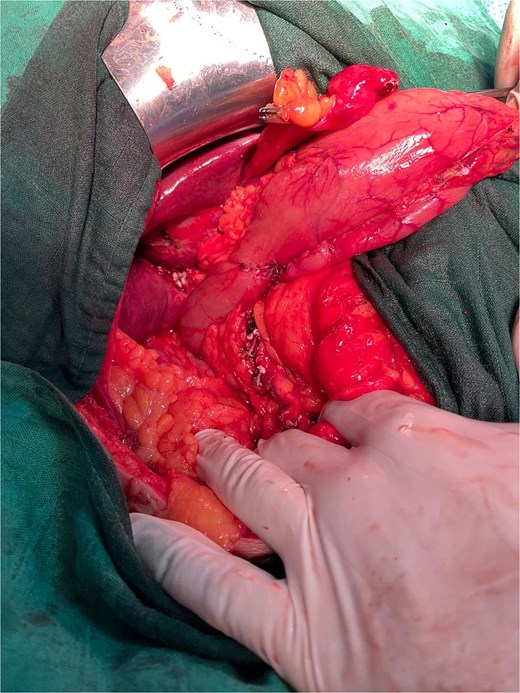
The initial laparoscopic approach was converted to right subcostal laparotomy (Fig. 2) due to unfavorable local conditions and severe inflammatory changes.

Surgical exploration revealed the true pathology: acute complicated cholecystitis with gallbladder fistulization to the subserosal gastric wall in the antro-pyloric region (Fig. 3), without mucosal involvement. The apparent ‘second gallbladder’ on imaging was actually a pseudocystic formation created by the fistulous communication and inflammatory process. The area was surrounded by significant inflammatory adhesions involving the omentum, creating a complex inflammatory mass.

Intraoperative view showing cholecystitis of a sclerotic and atrophic gallbladder associated with a cholecysto-gastric fistula.
Meticulous dissection allowed liberation of the gallbladder and separation of the pseudocystic gastric formation, with aspiration of purulent content from both the gallbladder and the fistulous tract. Antegrade cholecystectomy was performed with clipping and division of the cystic artery and duct. The fistulous tract was carefully dissected, and partial resection of the affected gastric wall was completed (Fig. 4), followed by closure with 3–0 PDS suture, preserving the gastric mucosa integrity (Fig. 5).

Intraoperative image after resection of the gallbladder and the subserosal gastric cyst.
Frozen section examination of the gallbladder wall fragment showed no evidence of malignancy. The postoperative course was uneventful without complications. Definitive histopathological examination confirmed acute ulcerative and phlegmonous lithiasic cholecystitis with fistulous tract formation, without malignancy criteria.
Discussion
This case highlights the diagnostic complexity that can arise when inflammatory complications of gallbladder disease create unusual imaging appearances. The initial radiological interpretation suggested double gallbladder, a rare congenital anomaly that would have significant implications for surgical planning [6]. However, surgical exploration revealed that the apparent anatomical variant was actually a consequence of inflammatory fistulization.
Cholecystoenteric fistulas develop through a well-described pathophysiological process involving acute inflammation, ischemic necrosis, and subsequent perforation of the gallbladder wall with adherence to adjacent organs [7]. The gastric location, while less common than duodenal fistulization, can create particularly complex imaging findings due to the gastric wall’s capacity to form pseudocystic structures around the fistulous communication [8].
The diagnostic challenge in this case was multifaceted. First, the imaging suggested possible malignant transformation, which is a recognized risk in chronic cholecystitis and can significantly alter treatment approach [9]. Second, the apparent double gallbladder anatomy would have required specific surgical considerations for safe management of potentially duplicated biliary structures [10].
Magnetic resonance cholangiography, while considered the gold standard for biliary anatomy assessment, can be limited in the setting of severe inflammation where tissue planes become obscured and fistulous communications create complex fluid collections [11]. The ability of inflammatory processes to mimic anatomical variants underscores the importance of maintaining high clinical suspicion and readiness for intraoperative findings that may differ significantly from preoperative imaging.
The surgical management required conversion from laparoscopy to open approach, which is not uncommon in complicated gallbladder disease with conversion rates reaching 15%–20% in cases with severe inflammation [12]. The decision for conversion was appropriate given the complexity of the inflammatory process and the need for safe dissection of the fistulous tract while preserving gastric wall integrity.
This case emphasizes several important clinical points: the limitation of imaging in differentiating inflammatory complications from anatomical variants, the importance of maintaining surgical flexibility when preoperative and intraoperative findings diverge, and the need for experienced surgical judgment in managing complex inflammatory conditions.
Conclusion
This case demonstrates how acute cholecystitis complicated by biliary-gastric fistula can create imaging appearances mimicking rare anatomical variants such as double gallbladder. The diagnostic challenge lies in distinguishing between true anatomical variants and inflammatory pseudoformations. While advanced imaging techniques provide valuable information, surgical exploration remains crucial for definitive diagnosis and appropriate management. This case contributes to understanding the complex presentations of cholecystoenteric fistulas and emphasizes the importance of maintaining diagnostic flexibility in complicated biliary disease.
Conflict of interest statement
None declared.
Funding
None declared.



