-
PDF
- Split View
-
Views
-
Cite
Cite
Oren Gal, Ariel Polonsky, Shaul Pery, Unveiling the nature of a peritoneal implant using endoscopic ultrasound, Journal of Surgical Case Reports, Volume 2025, Issue 7, July 2025, rjaf504, https://doi.org/10.1093/jscr/rjaf504
Close - Share Icon Share
Abstract
Ovarian cancer is one of the leading causes of cancer deaths in women with a median age of diagnosis of 63. Commonly, late presentation leads to advanced disease with peritoneal involvement. Often, ovarian cancer recurs even after extensive surgical interventions and oncological therapy. Below, we present a case of a 75-year-old women with past surgical history of ovarian carcinoma who underwent debulking surgery and adjuvant chemotherapy treatment. During gynecological oncology follow-up positron emission tomography (PET-CT) scan she was diagnosed with fluorodeoxyglucose (FDG) uptaking, 12 mm lesion in the serosal surface of the recto-sigmoid junction. Due to the uncommon site of the lesion and its unknown histological nature, the lesion was biopsied during trans-rectal endoscopic sonography which held bases for further surgical intervention.
Introduction
Ovarian cancer is the fourth most common cause of female cancer death in the developed world with 220 000 new cases yearly worldwide. Commonly, late presentation leads to advanced disease with peritoneal involvement. The management of ovarian cancer requires cooperation of gynecological surgeons, oncologists, radiologists, pathologists, and palliative care specialists [1]. Debulking surgery, also called cytoreductive surgery, is a resection of the tumor as much as possible and an intended incomplete resection for unresectable malignant tumors. Optimal debulking surgery is considered as a surgery with maximal residual lesion size <1 cm. ovarian cancer is the cancer in which debulking surgery is most frequently conducted at present [2]. Following this surgery, continued follow-up is required, at times with need for a secondary debulking surgery.
Here, we present a case of a solitary 12 mm lesion with FDG uptake found on the serosal surface of the recto-sigmoid junction during a PET-CT scan performed 2 years after an index debulking surgery for metastatic ovarian carcinoma.
Case report
A 75-year-old woman with a past surgical history of serous papillary ovarian carcinoma underwent complete debulking surgery and adjuvant chemotherapy treatment 2 years prior to her current presentation. During follow-up, increased FDG uptake along with a 1.2-cm mass was seen on a PET-CT on the serosal surface of the recto-sigmoid junction (Fig. 1). An attempt was made to evaluate the lesion using trans-rectal sonography. Radial sonographic view showed a 12 mm, hypoechoic, well-defined lesion located at the serosal surface of the recto-sigmoid junction (Fig. 2). After reverting to a linear view, the lesion was sampled with fine-needle biopsy (Fig. 3) and whitish thick cores were retrieved (Fig. 4). The procedure was uneventful and no adverse events were noted. Pathology revealed fragments of high grade serous carcinoma of tubo-ovarian origin. Relying on the histological information gained from the biopsy, it was known that the lesion although not obvious to the eye during surgery, had to be found and resected. The surgical procedure was challenging with multiple adhesions, which made it difficult to locate the lesion. Based on the valuable preoperative knowledge, the patient was able to have a complete debulking of the tumor mass.
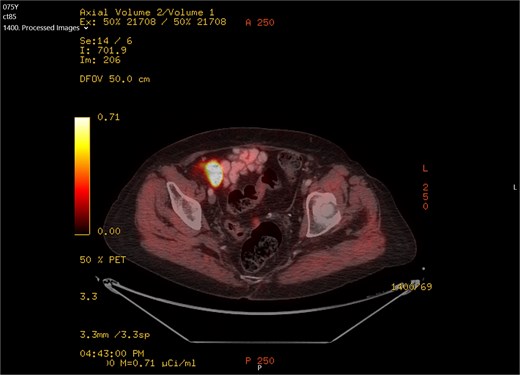
PET-CT scan showing FDG uptake at the recto-sigma junction seen as small bright spot in the middle of the screen.

Radial sonographic view of the malignant lesion at the 2 o'clock position.

Linear view of the malignant lesion seen as a hypoechoeic mass with biopsy needle inside.

Whitish core material obtained by fine-needle biopsy embedded on a slide before submission to pathological evaluation.
Discussion
Endoscopic ultrasound (EUS)-guided transmural biopsies are common practice in upper gastrointestinal (GI) and pancreatic lesions; however, more rare when it comes to the lower GI tract, especially proximal to the rectum [3]. The widespread use of colonoscopy has led to an increasing number of subepithelial lesions found in the colon incidentally. Those lesions are not accessible to normal endoscopic mucosal biopsy and hence led the way for lower GI tract endosonography. EUS enables differentiation between the GI wall layers, characterization of size, complexity, vasculature, and density of the lesion, as well as tissue acquisition [4]. The use of EUS and the recent development of forward-viewing echoendoscopes and through the scope EUS mini probes allows for EUS imaging of lesions throughout the entire tortuous colon, assess perianal disease, and drain pelvic abscesses associated with IBD. EUS drug delivery mechanism and substances are in different stages of development [5].
Secondary debulking surgery may be considered in select patients with good response to first line chemotherapy, a limited number of recurrent disease sites and a good performance status [6]. This treatment can prolong patient survival as well as palliate morbidity associated with advanced disease.
In the aforementioned case, we describe a unique situation in which the field of invasive gastroenterology had come to the help of gynecological oncology by an uncommon, yet elegant examination which lead the way to a second debulking surgery and improvement of oncological care. It is interesting to see if the field of invasive gastroenterology will enable EUS transmural diagnosis of other extra-colonic malignancies in the future.
Conflict of interest statement
None declared.
Funding
No financial support was given for the reported case.
References
- positron-emission tomography
- fluorodeoxyglucose f18
- ultrasonography
- debulking
- adjuvant chemotherapy
- endoscopy
- fine needle biopsy
- follow-up
- surgical procedures, operative
- diagnosis
- peritoneum
- ovarian cancer
- computed tomography/positron emission tomography imaging
- surgical history
- carcinoma, ovarian epithelial
- gynecological oncology
- cancer death rate
- endoscopic ultrasound
- implants



