-
PDF
- Split View
-
Views
-
Cite
Cite
Hui Wen Chua, Natasha R T Lim, Allen W J Wong, Breast cancer masquerading as siliconoma: a cautionary tale, Journal of Surgical Case Reports, Volume 2025, Issue 7, July 2025, rjaf480, https://doi.org/10.1093/jscr/rjaf480
Close - Share Icon Share
Abstract
Free silicone injections to the breast for augmentation purposes have been prohibited in many countries but late complications are still seen. These complications can range from swelling to pain and breast lumps. We report a case of delayed diagnosis of cancer due to the presence of silicone granulomata in a patient. She subsequently underwent nipple-sparing mastectomy with immediate deep inferior epigastric perforator flap reconstruction with good oncological and cosmetic outcomes.
Introduction
Injection of foreign materials like liquid silicone, paraffin and gels have been used for breast augmentation since the 1940s. The high rate of complications like infection, migration, granuloma formation, chronic pain, and skin necrosis has led to the ban of this procedure in many countries [1, 2]. Despite this, free silicone injections are performed in some countries due to ease of performance with immediate results. Complications from such procedures are still seen. Moreover, silicone in breasts decreases the sensitivity of detecting cancer in conventional imaging modalities like mammography and ultrasound [3]. We report a case of delayed diagnosis of cancer due to the presence of silicone granulomata in a patient.
Case presentation
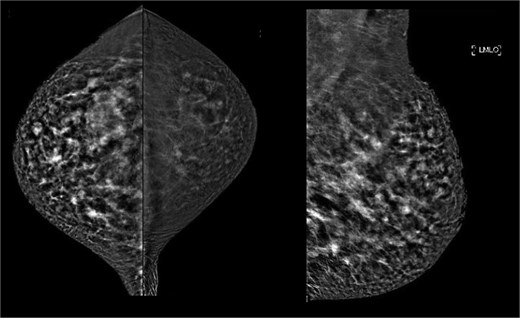
This was a 49-year-old lady of Philippine descent with previous free silicone injections in bilateral breasts in 1996. She was seen in the breast surgery clinic in October 2015 for a right breast lump in the upper outer quadrant. Mammogram showed extremely dense bilateral breasts with multiple dense oval opacities compatible with free silicone (Fig. 1). Ultrasound revealed a snowstorm appearance, with round cystic lesions scattered throughout both breasts representing silicone granuloma (Fig. 2). She was reassured at the time.
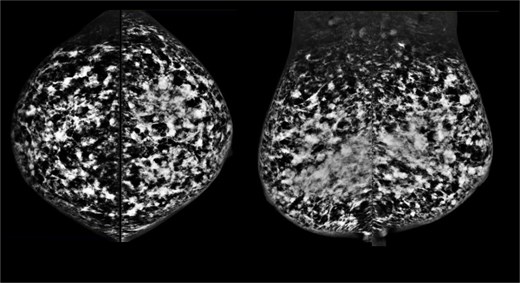
October 2015: Mammography images; craniocaudal views (left), mediolateral oblique views (right).
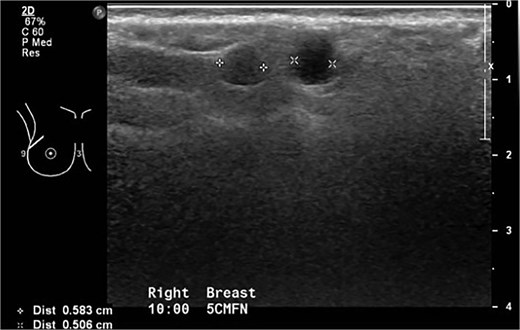
October 2015: Ultrasonography showing snowstorm appearance secondary to free silicone injection, with round cystic lesions scattered throughout both breasts representing silicone granuloma.
She re-presented in August 2020 with the same complaint. Ultrasound showed marked snowstorm appearance secondary to silicone injection (Fig. 3). This obscured ultrasound visualization and limited assessment and interpretation. On additional contrast-enhanced spectral mammography (CESM), background high density silicone deposits and granulomata affected the acquisition of right mediolateral oblique view. On the right craniocaudal view, there was a suggestion of a 44 × 34 mm faint enhancing mass in the lateral half of the right breast, with lobulated and partly obscured margins (Figs 4 and 5). This corresponded to the palpable lump and represented a cluster of silicone deposits and granulomata but malignancy could not be excluded. She underwent core biopsy of the lump and histology showed chronic histiocytic inflammation suggestive of silicone related reaction. She was given analgesia for symptomatic relief.
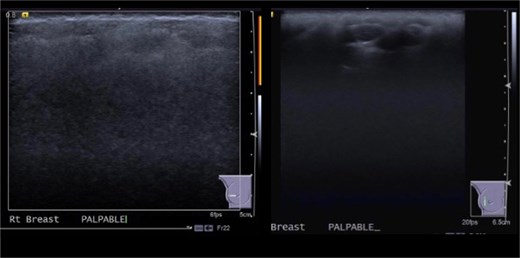
August 2020: Ultrasonography images showing marked snowstorm appearance secondary to silicone injection with multiple silicone deposits and granulomata in superficial breast tissue.
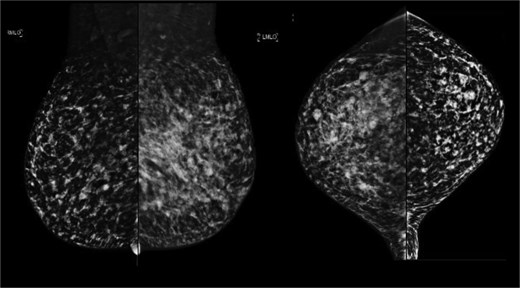
August 2020: Mammography images: Mediolateral oblique views (left), craniocaudal views (right).
August 2020: Limited contrast enhanced spectral mammography showing enhancing mass in lateral half of right breast (right mediolateral oblique view not available—Mammogram machine unable to expose despite repeated attempts).
In June 2021, after 6 months of the breast lump increasing in size and pain, she sought a second opinion. Examination showed a firm and mobile right breast mass 120 × 80 mm from 6 to 11 o’clock position. Repeat ultrasound showed diffuse ill-defined hyperechoic areas with posterior shadowing throughout the right breast, with superficially located cystic areas, in keeping with silicone granulomata and oil cysts (Fig. 6). A superficially located ill-defined hypoechoic area measuring 43 × 14 × 32 mm corresponded to the palpable lesion. Several right axillary lymph nodes were hyperechoic with posterior shadowing in keeping with silicone deposition. Magnetic resonance imaging (MRI) breast was offered given the non-diagnostic routine imaging, along with option of excision biopsy of the enlarging symptomatic lump.
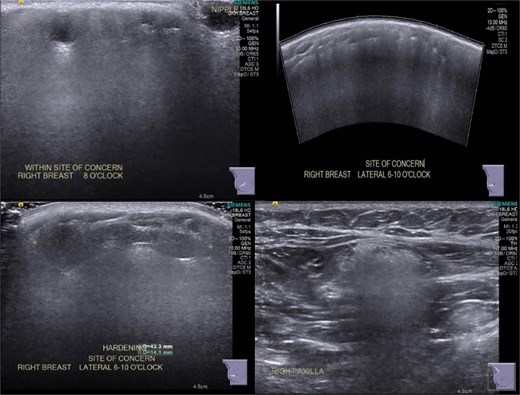
June 2021: Repeat ultrasonography showing silicone granulomata.
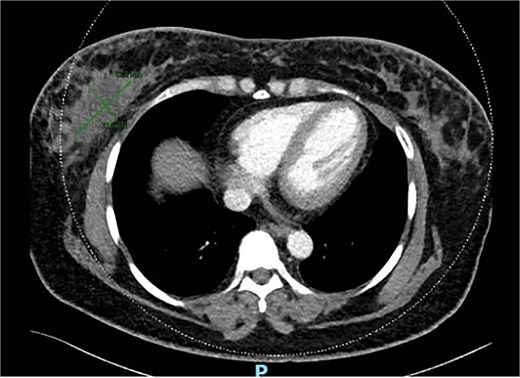
She underwent excision biopsy of the 80 mm right breast siliconoma in Aug 2021. Histology showed 80 mm invasive mammary carcinoma with apocrine component. GATA 3 positive, CK7 positive. Estrogen receptor (ER) and progesterone receptor (PR) negative and cerB2 positive. Margins were involved anteriorly, superiorly and posteriorly. Staging computed tomography (CT) scan showed multiple nodules scattered in both breasts and post-surgical seroma including a lobulated and enhancing soft tissue in retro-areolar region (Fig. 7). No metastasis noted.
MRI breast showed seroma from excision biopsy and delayed enhancement in the anterior aspect of the collection that may represent residual disease (Fig. 8). She underwent breast conserving surgery to obtain clear margins, and sentinel node biopsy. Wide excision histology showed residual 13 mm invasive carcinoma with clear margins and one lymph node positive on sentinel node biopsy. She subsequently underwent axillary clearance and completion nipple-sparing mastectomy and reconstruction with free deep inferior epigastric perforator (DIEP) flap (Fig. 9). Histology revealed no residual carcinoma and further nodal metastasis. She underwent adjuvant chemotherapy, targeted therapy and radiotherapy. She has remained well 3 years after her surgery and continues to be screened for cancer annually with a MRI for her contralateral breast.
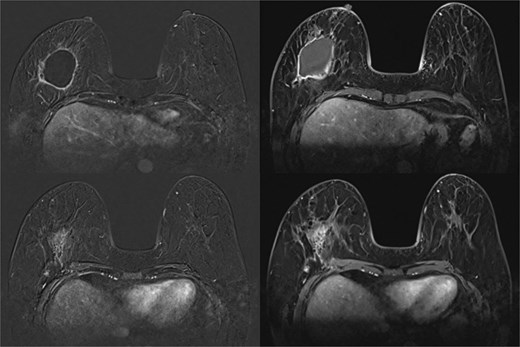
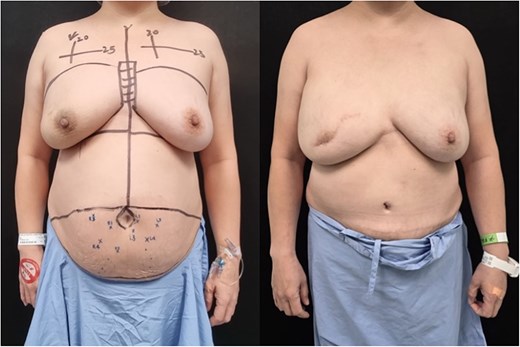
Photo taken before nipple-sparing mastectomy and DIEP flap reconstruction (left); taken 1 year after surgery (right).
Discussion
Complications can arise immediately and much later after injection. This patient developed symptoms 9 years after and conventional imaging modalities only identified the presence of silicone. MRI is a more sensitive modality in detecting cancers in patients with siliconomas [4–7]. Cancers can be missed without the appropriate imaging modality in such patients. CESM has been used since 2011 by utilizing the difference in attenuation coefficients of iodine and glandular tissues under low and high energy intermittent exposures to combine and re-create images that eliminate background tissue [7]. The sensitivity of CESM ranges from 93%–100%, with specificity at 63%–88% [8]. A systematic review and meta-analysis by Shahraki et al. showed that CESM has higher specificity, positive predictive value and diagnostic confidence rate than MRI [9]. This is however based on normal breasts without free silicone injection.
Besides considering MRI, one should have a low threshold to get histological diagnosis to ensure cancer is not missed, especially in symptomatic patients. A full excision biopsy should be performed if there is clinical-histological discordance.
There is no management consensus in patients with silicone injections for prophylactic mastectomy. In a case series of 28 patients by Parsons et al., nipple-sparing mastectomy with delayed reconstruction was recommended in patients who had developed complications [11]. Delayed reconstruction was due to concerns of bleeding due to intense inflammation and reconstruction was performed with tissue expanders [10]. Despite extensive inflammation in the normal tissue planes caused by the silicone granuloma, we were able to perform successful immediate reconstruction with autologous free DIEP flap after nipple-sparing mastectomy. Siliconomas are prone to recurrent infection, and the use of well vascularised flaps such as the DIEP flap remain as a good safeguard against infection and support favourable oncologic and cosmetic outcomes [12].
Conclusion
This case underscores diagnostic pitfalls associated with free silicone injections to the breast, where foreign body granulomata obscures conventional imaging and masks underlying malignancy. It is important that care providers are vigilant in the treatment of these patients. The threshold to considering advanced imaging and tissue diagnosis should be lower in such patients. This case also demonstrates that immediate autologous reconstruction using a well-vascularized DIEP flap following nipple-sparing mastectomy is feasible and safe in patients with siliconomas.
Conflict of interest statement
None declared.
Funding
None declared.



