-
PDF
- Split View
-
Views
-
Cite
Cite
Sobia Yasmeen, Obaid Ur Rahman, Hassan Tahir, Rabia Anwar, Muhammad Imran Khan, The median artery forearm free flap: an anatomic anomaly transformed into a surgical opportunity, Journal of Surgical Case Reports, Volume 2025, Issue 7, July 2025, rjaf433, https://doi.org/10.1093/jscr/rjaf433
Close - Share Icon Share
Abstract
Upper limb anatomical anomalies and variation are common and have frequently been documented in literature. As forearm is a common site for flap harvest, these anomalies play a critical role in planning, designing, and harvesting a flap. We planned an ulnar forearm flap for head and neck reconstruction. During flap harvest, it was noted that there is a persistent median artery supplying perforators to ulnar side skin and ulnar artery was absent. We then modified our design and based our free flap on median artery. This case report describes this free median artery flap utilized for head and neck reconstruction.
Introduction
Upper limb arterial anatomical variations are relatively common, with the literature documenting various combinations of the arterial system [1]. While these variations typically hold limited clinical significance, they become important when harvesting a forearm flap. Radial [2] and ulnar forearm [3] are widely recognized as valuable reconstructive options and the reconstructive surgeons must be aware of the potential arterial anomalies encountered during flap harvesting [4]. This knowledge allows for better customization of flap planning, design, and harvesting techniques. The persistent median artery, though rare [5], can play a crucial role in forearm flap planning. In our case, we successfully raised a free flap based on the median artery, as the ulnar artery was absent and the hand was perfused via the radial artery.
Case report
A young male patient with a history of a gunshot injury to the face, resulting in tissue loss and disfigurement, previously underwent an anterolateral thigh free flap for wound coverage. He is now admitted for lip and cheek reconstruction. An Abbe-Estlander flap was planned for lip reconstruction, and an ulnar forearm free flap for the cheek defect, due to the potential for non-hair-bearing skin at the site.
Preoperatively, Allen's test revealed the radial artery as the dominant supply to the hand, with the ulnar artery contributing weakly. Doppler examination identified two perforators on the volar-ulnar aspect, medial to the flexor carpi ulnaris (FCU). The flap was planned over the volar-ulnar forearm, incorporating non-hair-bearing skin and the identified perforators (Fig. 1).

Photograph of preoperative markings and perforator identification.
Flap dissection began from the radial to ulnar side. Two perforators were identified distally, but their course directed toward the radial side which was unusual. Dissection was shifted proximally in the subfacial plane, the FCU was retracted, and it was noted that the ulnar artery was absent, though the ulnar nerve remained in its usual position (Fig. 2). The identified perforators were traced to the median artery, which was present alongside the median nerve and splitting the palmaris longus into two halves (see Supplementary Video S1).

Photograph showing absent ulnar artery, intact ulnar nerve, and perforators running from median artery to the skin.
The radial artery was identified and preserved (Fig. 3). Flap was designed to be based on the median artery perforators, and a medial incision was made. The palmaris longus was divided and partial dissection of the flap and median artery was performed (Fig. 4). The tourniquet was released, and a clamp placed on the median artery distal end to confirm hand perfusion through the radial artery and flap perfusion through the median artery. After confirming, both the distal median artery and accompanying venae commitantes were divided, and the flap was raised proximally (see Supplementary Video S2). The proximal part of the median artery, arising from the radial artery after the interosseous branch was cut.


Photograph showing dissected median artery and divided palmaris longus tendon.
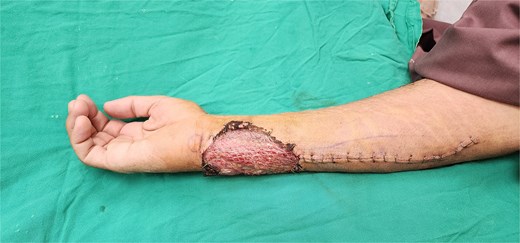
The flap was transferred to the neck, where anastomosis was performed with the facial artery and vein. The donor site was covered with a split-thickness skin graft (Fig. 5). Both the flap and skin graft healed uneventfully, with no hand function deficits postoperatively.
Discussion
The incidence of the median artery ranges from 1.1% to 27.1% [6] though it typically regresses by the 8th week of gestation [7]. When present, it arises from the ulnar, radial, or common interosseous artery and is of adequate caliber [8] and runs alongside the median nerve but may also penetrate it [7]. We have encountered it during various forearm explorations, often in cases of traumatic injury.
Forearm flap can be based on the ulnar or radial artery [9]. While typically harvested from the radial artery, the ulnar-based forearm flap may be preferred [10], as in our study, to utilize non-hair-bearing skin for facial reconstruction.
Numerous abnormal vascular patterns of the persistent median artery, including absent radial or ulnar arteries, have been reported [11]. Such anomalies may pose risks during flap harvest, to flap or hand vascularity [12]. Preoperative Allen's test, routinely done to assess vascular dominance [13], showed radial artery dominance in our case.
Niranjan and Shibu [8] reported a case of a pedicled radial forearm flap based on the median artery for post-burn wound coverage. In 2008, Varley et al. [12] encountered the median artery while harvesting a radial forearm free flap for head and neck reconstruction, but based the flap on the radial artery, leaving the median artery intact.
In 2008, Acarturk et al. [14] reported during radial forearm flap harvest that the radial artery supplied the forearm skin through a small perforator, with the rest of the skin supplied by perforators from the median artery branching off the radial artery. The common interosseous artery also arose from the radial artery. The flap was based on the radial artery, with the median and common interosseous arteries preserved to maintain hand perfusion. The flap survived, and hand remained perfused.
We encountered a similar anatomical variation during ulnar forearm flap harvest, where the median artery was the primary supplier of the ulnar forearm skin. However, our case differed in that the ulnar artery was absent, while the radial artery was normal. We based our flap on the median artery.
In 2009, Davidson and Pichora [15] reported the first free flap based on the median artery, where the radial artery was vestigial with small caliber. In contrast, we present a similar forearm flap based on the median artery, but with an absent ulnar artery, and normal radial artery. This specific combination has not been reported before in the literature. The incidence of absent ulnar artery is <0.015% [16], and only one previous free flap [15] based on the median artery has been documented.
In conclusion, surgeons should be prepared for anatomical variations during forearm flap harvest and understand their implications for both the flap and donor site. Key principles for safe surgery include preoperative exams (Allen’s test, Doppler), careful dissection, intraoperative vascular assessment, and maintaining awareness throughout the procedure.
Conflict of interest statement
None declared.
Funding
None declared.
IRB/ethical review committee
Study exemption approved.



