-
PDF
- Split View
-
Views
-
Cite
Cite
Saleh Husam Aldeligan, Abdulaziz S AlQahtani, Abdullah Aljunaydil, Nashwa Alzahrani, Fadi Alakeel, Budur T Althobaiti, Areej Bokhari, Synchronous presentation of Hodgkin lymphoma and papillary thyroid carcinoma in a young patient: a case review, Journal of Surgical Case Reports, Volume 2025, Issue 6, June 2025, rjaf398, https://doi.org/10.1093/jscr/rjaf398
Close - Share Icon Share
Abstract
The synchronous occurrence of Hodgkin lymphoma (HL) and papillary thyroid carcinoma (PTC) in a young adult without prior radiation exposure is exceedingly rare. The diagnostic challenge arises in differentiating between lymph node metastases from PTC and HL involvement. The absence of clear protocols for managing such cases further complicates treatment. We report a 28-year-old male with a body mass index (BMI) of 44.3 kg/m2 who presented with progressive neck swelling over 2 years. Initial investigations, including fine-needle aspiration (FNA) and imaging, revealed concurrent diagnoses of PTC and HL. The patient underwent total thyroidectomy with central compartment lymph node dissection, followed by radioactive iodine (RAI) ablation. Despite initial disease control, he later developed recurrent HL, confirmed via histopathological and immunohistochemical analysis. The coexistence of HL and PTC in a single patient raises questions regarding shared risk factors, though no established causal link exists. The rarity of this presentation highlights the necessity of a multidisciplinary approach for accurate diagnosis and treatment. Coordinating therapies such as RAI for PTC and chemotherapy for HL is critical to optimizing patient outcomes while minimizing adverse effects. This case underscores the importance of early recognition and tailored management of synchronous malignancies. The lack of established guidelines necessitates documentation of such cases to inform future clinical practice. Further research into potential risk factors, including genetic predisposition and environmental influences, is warranted.
Introduction
The synchronous occurrence of Hodgkin lymphoma (HL) and papillary thyroid carcinoma (PTC) in a young adult without prior radiation exposure is infrequent. PTC accounts for 89.4% of thyroid cancers, while HL predominantly affects younger individuals [1, 2]. Most documented cases of such dual malignancies have been associated with radiation, a known risk factor for secondary cancers [2]. The co-presentation complicates diagnosis, as lymphadenopathy may represent HL or PTC metastasis, making accurate differentiation essential [2, 3]. Synchronous malignancies constitute ⁓6% of global cancer cases, with a reported prevalence ranging from 2.15% to 17.2% [4, 5]. However, the concurrent presence of HL and PTC is particularly uncommon, lacking a clearly established etiological link between thyroid tumors and lymphomas [6, 7]. Risk factors for multiple primaries include genetic predisposition, environmental exposures, and prior treatments such as radiotherapy [5]. Effective diagnosis requires fine-needle aspiration (FNA) for PTC, lymph node biopsy for HL, and detailed imaging [computed topography (CT), positron emission tomography (PET), ultrasound (US)] to distinguish between metastatic and primary lesions [3]. Treatment typically involves thyroidectomy with or without radioactive iodine (RAI) for PTC and ABVD chemotherapy for HL, requiring coordination to avoid therapeutic overlap or toxicity [3, 5, 8]. Given the complexity of such cases, a multidisciplinary team (MDT) is crucial to guide individualized management and improve outcomes [9]. This case underscores the diagnostic and therapeutic challenges posed by synchronous HL and PTC in a radiation-naïve patient, highlighting the importance of clinical vigilance and collaborative care.
Clinical presentation
A 28-year-old man with a BMI of 44.3 kg/m2 and, a history of hypertriglyceridemia on gemfibrozil 600 mg complained of neck swelling for 2 years. It began as a nodular swelling at the right supraclavicular region and later spread to the right axillary and left supraclavicular areas. For one month, the patient had an unintentional weight loss of 4 kg and a few episodes of night sweats but no fatigue, fever, or compressive symptoms. He never received any radiation treatment. The family history was positive for an aunt with a malignant thyroid disease, for which she had a total thyroidectomy done. He was also on calcium carbonate 1200 mg orally thrice daily and levothyroxine 200 mcg orally once daily. On general examination, the patient did not look dehydrated, the patient was afebrile and did not appear to be in acute respiratory distress. There was a firm, nontender, nonmobile mass in the right anterior neck which represents lower cervical lymphadenopathy. No thyroid nodules, thrills, or shift of the trachea to the right were found. Abdominal examination was normal, that is, no enlargement or tender masses were felt on abdominal palpation. It started in January 2018 with right sided lymph node enlargement and a detailed assessment was done at a hospital in the United Kingdom (UK) in March 2020. FNA of the neck nodes showed features of HL and the thyroid US showed a hypoechoic nodule with punctate calcifications measuring 3.9 × 1.9 cm and TI-RADS 5. Other findings were bilateral clinically suspicious cervical lymphadenopathy; the largest nodes being 3.6 × 2 cm on the right side and 2.8 × 1.3 cm on the left side. The laboratory findings included T3 of 5.19 pmol/L, T4 of 25 pmol/L, and thyroid stimulating hormone (TSH) of 0.817μIU/ml. According to these observations, the patient underwent further investigations and imaging, CT of the chest revealed necrotic mediastinal, bilateral axillary, and subpectoral lymph nodes suggesting intrathoracic metastases most probably from PTC or lymphoma (Fig. 1). A nuclear medicine scan confirmed FDG-avid disease in the thyroid and nodal areas above the diaphragm. A subsequent FNA of the thyroid nodule revealed papillary thyroid carcinoma (Fig. 2). The patient had a total thyroidectomy, central compartment lymph node dissection, and excision in March 2020. Surgical pathology showed PTC in the right thyroid lobe measuring 2.5 cm in diameter and ipsilateral cervical lymph node involvement. The postoperative treatment included radioactive iodine ablation of 120 mCi in December 2020, and thyroglobulin level was negative. However, the patient got other symptoms by November 2023 after the above-mentioned interventions were conducted. Postoperative US of the neck, done after thyroidectomy, did not demonstrate any thyroid tissue but multiple enlarged cervical lymph nodes, including one that was 2.3 × 1.2 cm in size, with some of the nodes matted and non-encapsulated with loss of fatty hilum. CT imaging revealed an interval increase in the size of right cervical and supraclavicular LN (Fig. 3) and nuclear imaging showed relapsed HL with FDG-avid lymph nodes, above and below the diaphragm. The histopathological examination of the right cervical lymph node excisional biopsy was done and immunohistochemistry staining of markers compatible with CHL was observed (Figs 4 and 5). The tumor cells were positive for CD 30, CD 15 (partially), MUM 1, and PAX 5 (faintly), and the reactive lymphocytes for CD 3 only. The diagnosis of relapse of classical Hodgkin lymphoma (CHL) called for additional oncologic assessment and intervention.

Bilateral enlarged and necrotic left intraparotid, cervical, and supraclavicular lymph nodes.
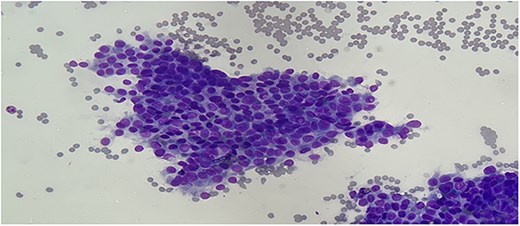
Differentiation quick staining of the thyroid FNA showing cytologic features of classic papillary thyroid carcinoma: oval enlarged nuclei, with nuclear overlapping, intranuclear grooves, and intranuclear cytoplasmic pseudoinclusions (original magnification ×400).

Post-total thyroidectomy and bilateral neck dissection with no signs of recurrence or residual at the thyroid bed. There is a right level IV 11 mm lymph node near the clip of neck dissection.
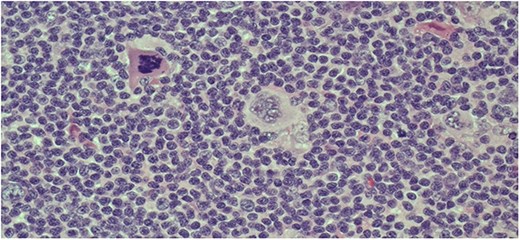
Hematoxylin and eosin staining of the lymph node biopsy showing the presence of large atypical Reed-Sternberg cells (original magnification ×200).
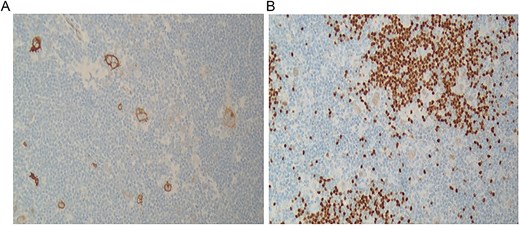
Immunohistochemical staining of the lymph node showing positivity for CD30 (original magnification ×100) (A), and PAX-5 (dim) (original magnification ×400).
Discussion
HL and PTC are rare malignancies that can coexist in young adults; no data regarding radiation exposure has been reported in the previous reports. Of the thyroid cancers, PTC is the most frequent and HL primarily affects the young population making the combined presentation diagnostic and therapeutic enigmas. Discriminating lymph node metastases derived from PTC and involvement of HL constitute a significant diagnostic challenge despite the inherently distinct histopathological characteristics of these two diseases. The implications of such synchronous cancers underscore no common risk factors to tie these malignancies and a paucity of well-defined approaches to managing them. A team approach embraced in its development reflects well-harmonized care provision which aims at enhancing diagnostic accuracy as well as individualized treatment planning. Reporting such cases contributes to sharpening the picture of the clinical process of synchronous malignant neoplasms and developing approaches to managing similar cases in the future. This opportunity supports the use of the MDT in the management of patients diagnosed with PTC because it increases compliance with clinical guidelines and allows for patient-centered care plans based on the patient’s profile [10]. It also emphasizes the significance of histopathological assessment in this case [1]. However, the management of synchronous HL and PTC is very complicated due to the hermeneutics of the diagnostic tools and the treatment strategies. If there is a conflict between the FNA cytology of a lymph node where HL and PTC metastases cannot be differentiated, then further pathological and immunohistochemical evaluation is required to arrive at a correct diagnosis [1]. Other treatment challenges are added in concurrent cancers especially when treating them with modalities like RAI in PTC and chemotherapy (ABVD) in HL. From these treatments, it is obvious that these treatments have to be strictly harmonized to avoid many kinds of interactions and to achieve the best results for the patient [1–12]. Also, the lack of evidence due to the low frequency of synchronous HL and PTC is a real problem. The lack of well established guidelines and definitive long term follow up information allows for presenting these cases mostly as descriptive data [1]. Furthermore, RAI therapy for thyroid cancer has been found to increase the incidences of secondary malignancies including hematological cancers thus the need to consider the risk benefit ratio carefully in management [12–14]. Now, HL and PTC have not been postulated to have solidified causal factors but might be associated with obesity, genetic susceptibility, and early environmental imprinting. There is evidence that suggests that obesity is connected with increased thyroid cancer risk and the relative risk rate of obesity to non obesity is 1.55 times [15]. By presenting this unusual example, we hope to increase knowledge of synchronous malignancies, improve the approach to management, and add to the educational literature.
Conflict of interest statement
None declared.
Funding
None declared.
References
- body mass index procedure
- cancer
- chemotherapy regimen
- radiation exposure
- fine needle biopsy
- hodgkin's disease
- genetic predisposition to disease
- lymphoma
- thyroidectomy
- diagnosis
- diagnostic imaging
- guidelines
- lymph node dissection
- radioactive iodine
- lymph node metastasis
- cervical lymph node group
- thyroid carcinoma, papillary
- ablation
- young adult
- central compartment
- neck swelling
- histopathology tests



