-
PDF
- Split View
-
Views
-
Cite
Cite
Rasheed Elayyan, Rebaz Abdullah, Tani Fasih, Supraclavicular lymphadenopathy: an unexpected consequence of breast implant rupture, Journal of Surgical Case Reports, Volume 2025, Issue 5, May 2025, rjaf308, https://doi.org/10.1093/jscr/rjaf308
Close - Share Icon Share
Abstract
Supraclavicular lymphadenopathy is a rare manifestation of silicone lymphadenopathy, a complication arising from breast implant rupture. We present a case of a 39-year-old woman with a history of bilateral breast augmentation using Poly Implant Prothèse implants who developed left breast swelling and progressive supraclavicular lymphadenopathy. Imaging revealed rupture of the left implant with silicone migration to supraclavicular lymph nodes, confirmed by the characteristic “snowstorm” sign on ultrasound. Surgical intervention involved bilateral implant removal and partial capsulectomy, with histopathological evaluation showing benign findings. Silicone lymphadenopathy, though typically associated with axillary nodes, can extend to cervical region posing diagnostic challenges. This case highlights the importance of considering silicone lymphadenopathy in patients with unexplained cervical lymphadenopathy and a history of breast implants. Diagnostic imaging and patient-centered management strategies remain crucial in addressing this rare but significant condition.
Introduction
Cervical lymphadenopathy is mostly attributed to local infectious or malignant process within its field of drainage. Cervical lymph nodes, including the supraclavicular nodes, drain regions such as the head, neck, breast, and upper abdomen, making them potential sites for malignancies originating from any of these areas [1]. For example more than a third (37.5%) of chest pathologies have the potential to metastasize to the cervical lymph nodes [2].
Breast augmentation is the most common cosmetic surgical procedure in the United Kingdom, with around 7000 cases recorded in 2022 [3]. The history of breast implants for augmentation began with the first silicone gel breast implant by Cronin and Gerow in 1964, marking the modern era [4]. This early implant was a thin-shelled device filled with low-viscosity silicone. Over the years, silicone implants evolved, with various brands and designs entering the market. However, Poly Implant Prothèse (PIP) implants were withdrawn in 2010 due to the use of industrial-grade silicone, which had a rupture rate up to 30 times higher than other implants [5].
Silicone lymphadenopathy, which occurs as a foreign body reaction to silicone, is a well-known complication of breast augmentation with silicone-based materials. It arises when silicone particles migrate to the regional lymph nodes. This can happen due to implant rupture or the leakage of tiny amounts of silicone gel through the outer shell, a process called “gel bleed.” Most cases involve lymphadenopathy in the axillary or mediastinal regions, while reports of silicone-associated lymphadenopathy in the cervical region are very rare [6, 7]. The incidence of silicone lymphadenopathy is more common in women with (PIP) implants due to the known increased rates of rupture [8].
To our knowledge, there are only a limited number of reported cases of silicone cervical lymphadenopathy. We are reporting a case of supraclavicular silicone lymphadenopathy attributed to a breast PIP implant rupture. This case contributes to the limited evidence of cervical silicone lymphadenopathy and highlights the importance of considering it in the deferential diagnosis when evaluating neck lumps in patients with a history of silicone breast implants.
Case presentation
Patient presentation
A 39-year-old woman with a history of bilateral breast augmentation 16 years prior presented with progressive left breast swelling over 1 week. Examination revealed left breast asymmetry, with marked enlargement and firmness compared to the right. Palpable left axillary lymph nodes were noted. The patient denied fever, pain, systemic symptoms, or prior breast issues and reported no significant comorbidities.
Initial investigations
Ultrasound of left breast and axilla: Revealed rupture of the left implant with intracapsular and extracapsular leakage, along with echogenic peri-implant fluid. Enlarged axillary lymph nodes were visualized (Figs 1 and 2).
Fluid aspiration: Approximately 180 mL of serous-like fluid was aspirated. Cytology showed bland adipocytes, lymphoid cells, and debris without malignancy.
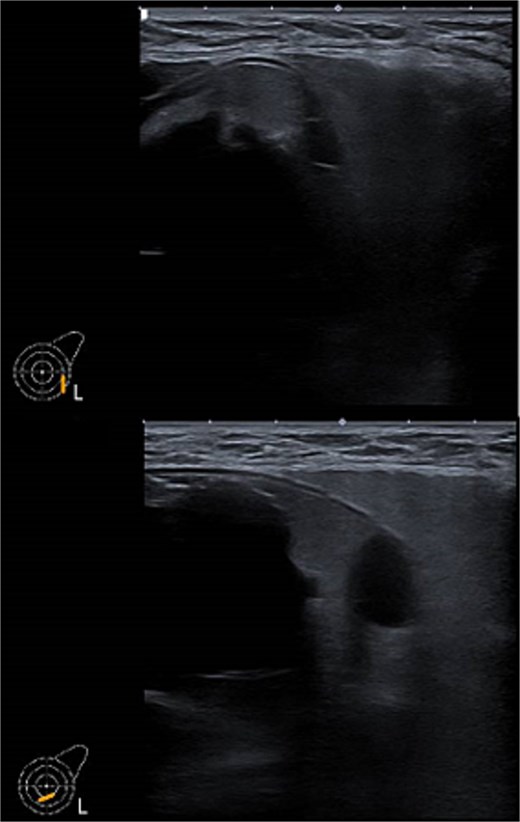
Ultrasound of the left breast showed rupture of the left breast implant with intracapsular and extracapsular leakage, surrounded by echogenic peri-implant fluid.
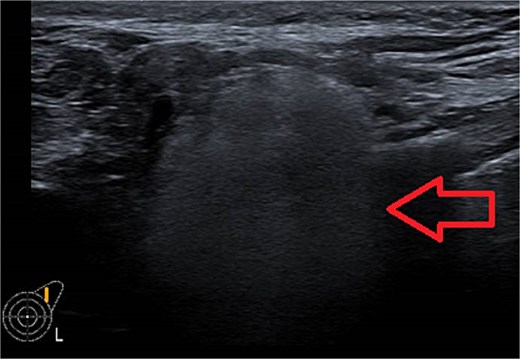
Ultrasound of the left axilla showed the typical appearance of the lymph node siliconoma.
The patient was scheduled for bilateral implant removal with or without capsulectomies.
Subsequent course
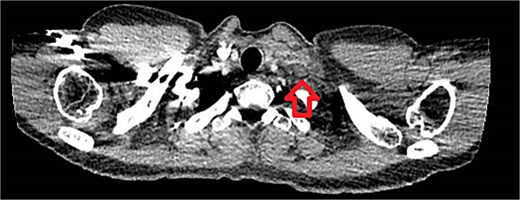
One week later, the patient reported a new lump in the left supraclavicular area. Examination revealed a 2 × 3 cm, nontender, mobile mass, confirmed by ultrasound to be silicone deposition (Figs 3 and 4). Increased breast swelling and lymphadenopathy were attributed to implant rupture and silicone migration.

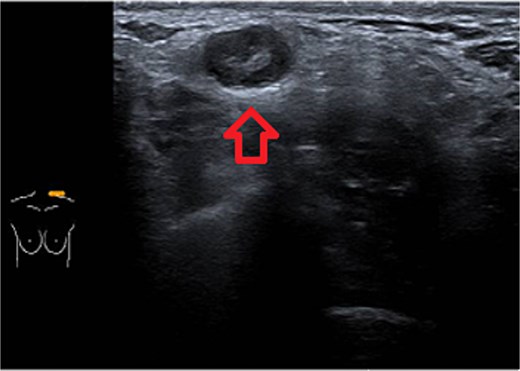
Typical snowstorm appearance of supraclavicular silicone lymphadenopathy.
Emergency presentation
The patient presented to the emergency department the same day with shortness of breath. Investigations were normal except for a mildly elevated D-dimer. A CT pulmonary angiogram excluded pulmonary embolism but confirmed the supraclavicular mass (Fig. 5). The patient was reassured and referred back to the breast clinic.
Surgical management
The patient underwent bilateral implant removal 2 weeks later.
Intraoperative findings:


A partial capsulectomy was performed on the left side due to poor dissection planes. Histopathology revealed benign features.
Discussion
Breast implants are regarded as a safe surgical option with minimal associated complications. Recent innovations in their design and new technologies have improved their safety, reliability, and acceptance [9]. Silicone lymphadenopathy is a breast implant complication characterized by the migration of silicone to surrounding soft tissues or lymph nodes. Silicone is transported to nearby lymph nodes by macrophages, where it initiates a foreign body reaction. This reaction causes chronic inflammation, eventually leading to lymphadenopathy [6].
A recent systematic review of 190 reported silicone lymphadenopathy areas showed that axillary lymphadenopathy was the most common, with 136 cases representing 72% of the cases, internal mammary lymphadenopathy in 40 case representing 21% of the cases, cervical/supraclavicular lymphadenopathy in 36 cases representing 19% of the cases, mediastinal in 24 cases representing 13% of the cases, and in 43 cases multiple nodal regions were involved representing 23% of the cases [10].
Imaging is a vital first step in the diagnostic evaluation of patients with lymphadenopathy. Ultrasound is the primary tool for diagnosing silicone lymphadenopathy, while additional imaging techniques, including MRI, CT, and mammography, can offer further insights for confirmation and detailed assessment of lymphadenopathy [11]. The sensitivity and specificity of using ultrasound to diagnose silicone lymphadenopathy by identifying the snowstorm sign have been reported as 87.5% and 100%, respectively [11]. In our case, the ultrasound typical snowstorm appearance was enough to make the diagnosis. Even though if any clinical concern about malignant or infectious process, cytological or histological evaluation is mandatory to confirm the diagnosis. Also in patients with previously treated breast cancer and having the implant as reconstructive measure; concerns about disease recurrence should be carefully considered.
The implant’s integrity should always be assessed, considering surgical intervention if rupture is identified. For enlarged lymph nodes, the key decision is excision or monitoring, made collaboratively with the patient. In our case, as the lymphadenopathy was asymptomatic with no compressive symptoms or recurrent inflammatory flare-ups, monitoring was chosen.
Conclusion
This case highlights the importance of considering silicone lymphadenopathy as a possible differential diagnosis in patients with supraclavicular adenopathy and a history of breast implants, particularly following implant rupture and when other causes are not identified. Otolaryngologists should take this pathology into account when there is diagnostic uncertainty in cases of isolated lymphadenopathy in the neck.
Conflict of interest statement
None declared.
Funding
None declared.
References
- edema
- ultrasonography
- rupture
- silicones
- surgical procedures, operative
- breast
- breast implants
- diagnosis
- diagnostic imaging
- cervical lymphadenopathy
- augmentation mammoplasty
- axillary lymph node group
- supraclavicular lymph node
- supraclavicular lymphadenopathy
- joint capsule excision
- implant removal
- histopathology tests
- implants
- lymphadenopathy
- rupture of breast implant



