-
PDF
- Split View
-
Views
-
Cite
Cite
LongHai Jin, Joel Budge, Falciform ligament cyst—a rare cause of abdominal pain, Journal of Surgical Case Reports, Volume 2025, Issue 5, May 2025, rjaf302, https://doi.org/10.1093/jscr/rjaf302
Close - Share Icon Share
Abstract
Falciform ligament is a fatty fibrous peritoneal fold located in the anterior abdomen. Falciform ligament cysts are rare, but they can cause significant symptoms and complications. A 38-year-old woman was diagnosed with an 8 cm falciform ligament cyst via ultrasound and computed tomography after presenting with chronic supraumbilical abdominal pain and a palpable abdominal mass. She underwent a laparoscopic resection of the cyst where the pathology subsequently confirmed the diagnosis. This article presents a literature review on the diagnosis and treatment of this rare pathological entity.
Introduction
Falciform ligament is a fatty fibrous peritoneal fold that runs down the anterior abdominal wall. Cysts rarely arise from the falciform ligament [1]. Lesions involving the falciform ligament should be carefully assessed to distinguish cysts from other more common differentials. This article reports a case of falciform ligament cyst and reviews the literature on this rare pathology.
Case
A 38-year-old woman presented to clinic with chronic supraumbilical abdominal pain. This was not associated with any gastrointestinal or constitutional symptoms, or systemic unwellness. She did not have any significant medical history. She had a Caesarean section 5 years prior. On examination, a large mass was palpated in the supraumbilical area; there was a small reducible fat-containing umbilical hernia, and there were no signs of peritonism. Blood tests including serum tumour markers were unremarkable. Computed tomography (CT) of the abdomen revealed an 8 × 3 cm hypodense lesion just deep to the anterior abdominal wall (Fig. 1). An ultrasound (USS) characterised this lesion as an 8 × 7 × 3 cm cyst with simple internal contents suggestive of a falciform ligament cyst (Fig. 2).
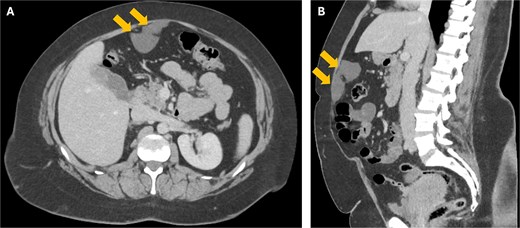
Axial (a) and coronal (b) CT images showing the 8 cm falciform ligament cyst (arrows) just deep to the anterior abdominal wall.

A USS image showing the 8 cm falciform ligament cyst with simple internal contents.
She underwent an elective resection of the falciform ligament cyst. Laparoscopic entry was established using an 11 mm Visiport in the left upper quadrant to avoid causing inadvertent injury to the cyst. Two 5 mm ports were placed under vision in the mid and lower left abdomen. The cyst was excised en bloc laparoscopically and retrieved through the left upper quadrant incision after it was lengthened (Fig. 3). The umbilical hernia was repaired laparoscopically using an intraperitoneal onlay mesh (Ventralex) with AbsorbaTack fixation. She was discharged home on the following day. Histopathology described a unilocular cyst that was lined by cuboidal epithelial cells with the wall composed of fibrocollagenous tissue; there were no malignant features. It was overall consistent with a benign falciform ligament cyst.
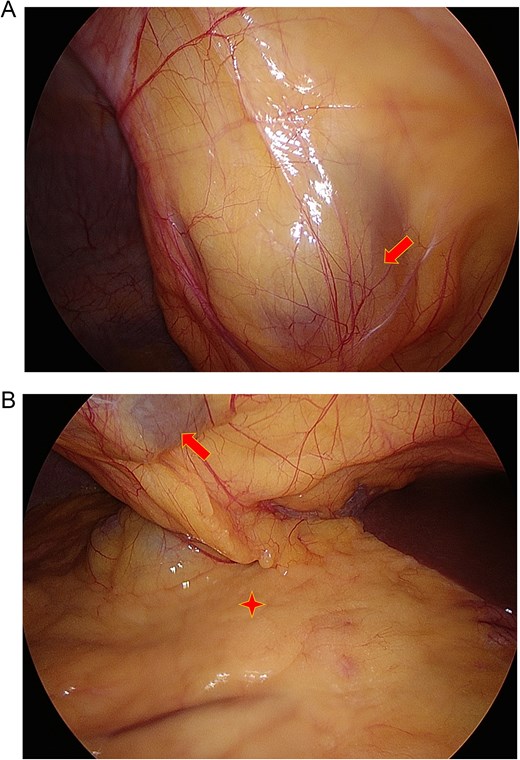
Intraoperative images showing the falciform ligament cyst (arrow) that was above and separate to the omentum (star).
Discussion
Falciform ligament is a fatty fibrous band that is formed by two adherent layers of peritoneum in the anterior abdomen [1]. It anchors the anterior surface of the liver to the anterior abdominal wall and spans from the inferior surface of the diaphragm to the umbilicus [1]. The inferior free edge of falciform ligament comprises ligamentum teres (round ligament of the liver), which contains the obliterated left umbilical vein [1]. Falciform ligament divides the liver morphologically into left and right lobes; however, the functional hepatic segments are defined by a different set of anatomical structures (Couinaud classification) [2]. Embryologically, falciform ligament is a remnant of the ventral mesentery [3].
Falciform cysts are incredibly rare; there have been only 18 cases reported in the literature to date [3, 4]. The mean age of the reported cases was 30.2 years (ranging from 4 months to 61 years); the male-to-female ratio was 1:1.2; and the mean cyst size was 10.5 cm. Although falciform cysts can be incidental findings; however, the most common symptom was abdominal pain [4]. Other reported symptoms include dyspepsia, abdominal distension, palpable mass or features of mass effect [4]. Falciform cysts can also develop complications such as cyst rupture, bleeding and torsion [3, 5].
The exact aetiology of falciform ligament cyst is unclear; primary and secondary causes have been suspected [3]. Falciform cyst may arise primarily from congenital mesenteric defect or failed obliteration of the umbilical vein; or they may develop secondarily following infection (bacterial or parasitic) or trauma [3, 6]. As falciform cysts are rare, other cystic differentials (e.g. urachal, choledochal, hepatic, omental, mesenteric, ovarian and renal), as well as tumour differentials (benign and malignant), should be considered. Blood test would typically include serum tumour markers. For imaging, CT and USS are the most frequently utilised modalities; magnetic resonance imaging has been utilised in some cases [3]. Percutaneous biopsy is not routinely performed due to concerns of cyst rupture and potential seeding to the biopsy tract. En bloc resection for pathology is the treatment of choice. Historically, resection of falciform cyst was accomplished via laparotomy (14 of 18 cases); laparoscopic resection has become the preferred approach over the last 15 years (4 cases) [3, 4]. All the cases achieved favourable outcomes following surgery without significant complications or recurrence.
Conclusion
Falciform ligament cysts are a rare pathological entity. Meticulous clinical assessment combined with imaging and biochemistry can help to differentiate falciform ligament cysts from other pathologies. Surgical resection is recommended to achieve pathological diagnosis as well as provide definitive treatment. Surgical advances have allowed a recent transition to laparoscopic resection with favourable outcomes.
Conflict of interest statement
None declared.
Funding
None declared.



