-
PDF
- Split View
-
Views
-
Cite
Cite
Mi-Jin Gu, Primary retroperitoneal mucinous cystic tumor with borderline malignancy: a case report and review of the literature, Journal of Surgical Case Reports, Volume 2025, Issue 5, May 2025, rjaf261, https://doi.org/10.1093/jscr/rjaf261
Close - Share Icon Share
Abstract
Primary retroperitoneal mucinous cystic tumor (PRMCT) is rare and preoperative diagnosis is challenging due to their rarity, lack of specific diagnostic imaging, clinical presentation, and tumor markers. We present an extremely rare case of PRMCT of borderline malignancy and summarize the characteristics of previously reported cases. Although the prognosis and optimal therapeutic strategies require further investigation due to its rarity, we should be considered when dealing with retroperitoneal cystic lesions.
Introduction
Primary retroperitoneal mucinous cystic tumors (PRMCT), including mucinous cystadenoma, mucinous cystic tumor of borderline malignancy (PBMCTB), and mucinous cystadenocarcinoma, are a very rare entity [1–3]. Since they are not commonly recognized, preoperative diagnosis is challenging. This case report aims to contribute to the understanding of this rare entity and to aid in making accurate preoperative diagnoses.
Case report
A 50-year-old female patient initially presented 3 years ago with uterine myoma. At that time, retroperitoneal enhanced computed tomography scan revealed multiple uterine myomas and an 8.0 × 5.8 cm lobulated cystic mass with smooth border in the left lower retroperitoneum (Fig. 1a). The cystic mass was suspected to be a retroperitoneal lymphangioma, and since there were no symptoms related to it, the patient decided to undergo observation rather than surgical removal. Since then, size, number, and feature of myomas and retroperitoneal mass showed no change in the follow-up annual CT (Fig. 1b). Recently, although the patient had no specific symptoms related to the cystic tumor, she felt that her abdomen was gradually becoming more bloated. As a result, she opted for surgical removal. The evaluation for serum tumor markers was not conducted. The surgically resected tumor was a large-sized, well-demarcated multilocular cyst with multifocal wall calcification, measuring 142 g and 10.5 × 6.8 × 4.5 cm. There were no ascites, lymphadenopathy, or adhesion to surrounding organs. Both ovaries were normal. The cyst contained clear mucinous fluid and showed focal papillary excrescences, measuring 2.4 × 2.0 cm. Microscopically, the cyst was mainly lined by a single layer of mucin-secreting columnar epithelium (Fig. 2a). In papillary excrescences, papillae lined by stratified mucinous epithelium with moderate nuclear atypia were observed (Fig. 2b). The tumor cells were positive for cytokeratin 7, and negative for cytokeratin 20 and calretinin. Ovarian-like stroma was found and showed positivity for estrogen receptor. No stromal invasion was found. Histologic diagnosis was PRMCTB. During a follow-up period of 24 months, there was no recurrence or metastasis.
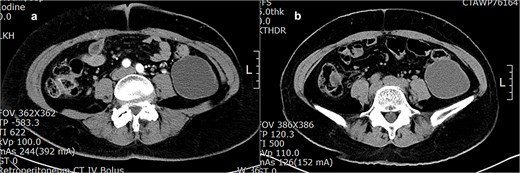
(a) Retroperitoneal enhanced CT shows a lobulated homogeneous cyst in the left lower abdomen. (b) A year later, there was no change in the size, shape, or characteristics of the cyst.
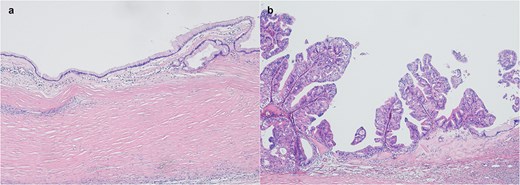
(a) Mucinous cystadenoma with a single layer of columnar epithelium with abundant intracellular mucin (HE, 4×). (b) PBMCTB shows papillary growth of stratified mucinous epithelium with nuclear atypia (HE, 4×).
Discussion
PRMCTs, including mucinous cystadenoma, PBMCTB, and mucinous cystadenocarcinoma are very rare entity and resemble ovarian mucinous cystic tumors [1–3].
Preoperative diagnosis of PRMCT is difficult due to the lack of specific clinical presentation, laboratory findings, or pathognomonic radiologic features [4]. Several hypotheses regarding the origin of PRMCT have been suggested but remain uncertain [2, 5–7]. The one is that PRMCT arises from ectopic ovarian tissue due to the histologic similarity with ovary mucinous cystic tumor. However, PRMCT has been reported in men and most of them did not contain ovarian tissue. Another is that PRMCT originates from teratoma or remnants of embryonal urogenital apparatus. However, the most widely accepted hypothesis is that PRMCT arises from invaginated peritoneal mesothelium, which undergoes subsequent mucinous metaplasia leading to cyst formation [2, 5].
We searched the reported cases of PRMCTB using PubMed and reviewed 28 cases without carcinoma component (Table 1). Including this case, twenty-three cases were women, and 6 were men. The median age was 43.8 years (22 to 68 years). The most common symptom was nonspecific abdominal pain and distension, and it predominantly appeared as a unilocular or multilocular cyst of variable size on imaging. Tumor markers, such as CA125, CA19-9, and CEA were not useful for diagnosis. Six cases revealed ovarian-like stroma, which suggests that female hormone may affect the development or growth of PRMCT [8]. All the tumors were removed through complete total resection, and their sizes ranged from 2 to 28 cm (mean, 14.96 cm). When reviewing the 29 reported cases so far, follow-up data for 20 patients were available, with an average follow-up period of 22.4 months (range: 1–148 months). During this period, one patient experienced a recurrence, and another patient had mediastinal lymph node metastasis. Due to the rarity and the lack of long-term follow-up data, it is difficult to determine the patient's prognosis of the PRMCTB. The management of PRMCTB is not yet well-established, but the best approach is complete surgical tumor removal. During surgery to remove the cystic mass, it is important to prevent rupture or spillage of cystic contents to reduce peritoneal dissemination and tumor recurrence [9]. Adjuvant chemotherapy after tumor resection also remains controversial. Some recommended just close follow-up, while others suggested treatment based on its histologically similar ovarian cancer [3, 4, 10, 11].
| Age/Sex . | Symptom . | Location . | Imaging finding . | Size (cm) . | Outcome (months) . |
|---|---|---|---|---|---|
| 41/F | Abdominal pain and tumor | ND | ND | 12 × 10 × 9 | NED (ND) |
| 38/F | Abdominal pain and distension | Left lower abdomen | Multilocular cyst | 11 | Mediastinal node metastasis (48 months) |
| 47/F | LUQ mass | Left upper quadrant | ND | 13 | ND |
| 63/M | Abdominal pain | Right kidney | Cyst | 11 | ND |
| 62/F | Abdominal pain | Right flank | Hypodense mass | 12 × 8.5 | NED (18 months) |
| 68/M | Right abdominal mass | Right abdomen | Cyst | 16 × 14.5 × 10 | NED |
| 65/F | Abdominal distension | Left abdominal cavity | Multilocular cyst | 21 × 14 | NED (12 months) |
| 32/M | Incidental on radiology | Around vena cava | ND | 7 × 6 × 4.4 | ND |
| 44/M | Abdominal pain | Interaortocaval | Multiple retroperitoneal mass | Multiple (2–5) | NED (12 months) |
| 35/F | Pelvic pain | Rear of the cecum | Cyst | 28 | NED (24 months) |
| 22/F | Abdominal pain | Superior of uterus | Cyst | 20 × 17.5 × 15 | NED (24 months) |
| 33/F | Abdominal pain, swelling | Left flank | Cyst | ND | NED (10 months) |
| 33/F | Tiredness | Descending colon | Cyst | 15 × 13 × 9 | NED (12 months) |
| 48/F | Postprandial fullness | Ascending colon mesentery | Cyst | 15 × 13 × 9 | NED (8 months) |
| 41/F | Flank pain | Right upper quadrant | Cyst | 21 × 16 | NED (18 months) |
| 31/F | Abdominal distension | Right retroperitoneal space | Multilocular cyst | 21 × 16 × 10 | ND |
| 36/F | Abdominal distension | Right lower abdomen | Cyst | 12 × 8 | NED (6 months) |
| 39/M | Back pain | Left pararenal space | Cyst | 6.9 × 4.4 | NED |
| 56/F | Painful urination | Right kidney | Multilocular cyst | 28 × 22 × 8 | Recur (6 months later) |
| 45/F | Abdominal pain | Left lower abdomen | Cyst with nodule | 15 | NED (12 months) |
| 25/F | Kidney mass | ND | Cyst with papillae | 15 | NED (148 months) |
| 43/F | Pelvic pain | ND | Cyst with papillae | 14 | NED (1 months) |
| 48/F | Enlarged mass | ND | Multilocular cyst | 7 | NED (34 months) |
| 37/M | Abdominal pain, mass | Right abdomen | Multilocular cyst | 22 × 11 | NED (12 months) |
| 26/F | Abdominal distension, pain | Left lower quadrant | Cyst | 13 × 10 × 8 | ND |
| 65/F | Mass | ND | Septate cyst | ND | NED (6 months) |
| 23/F | Mass | ND | Cyst | ND | ND |
| 68/F | Palpable abdominal mass | Left kidney | Multilocular cyst | 15 × 11 × 9 | NED (12 months) |
| 56/F (this) | Incidental on radiology | Retroperitoneum | Unilocular cyst | 8 × 5 | NED (24 months) |
| Age/Sex . | Symptom . | Location . | Imaging finding . | Size (cm) . | Outcome (months) . |
|---|---|---|---|---|---|
| 41/F | Abdominal pain and tumor | ND | ND | 12 × 10 × 9 | NED (ND) |
| 38/F | Abdominal pain and distension | Left lower abdomen | Multilocular cyst | 11 | Mediastinal node metastasis (48 months) |
| 47/F | LUQ mass | Left upper quadrant | ND | 13 | ND |
| 63/M | Abdominal pain | Right kidney | Cyst | 11 | ND |
| 62/F | Abdominal pain | Right flank | Hypodense mass | 12 × 8.5 | NED (18 months) |
| 68/M | Right abdominal mass | Right abdomen | Cyst | 16 × 14.5 × 10 | NED |
| 65/F | Abdominal distension | Left abdominal cavity | Multilocular cyst | 21 × 14 | NED (12 months) |
| 32/M | Incidental on radiology | Around vena cava | ND | 7 × 6 × 4.4 | ND |
| 44/M | Abdominal pain | Interaortocaval | Multiple retroperitoneal mass | Multiple (2–5) | NED (12 months) |
| 35/F | Pelvic pain | Rear of the cecum | Cyst | 28 | NED (24 months) |
| 22/F | Abdominal pain | Superior of uterus | Cyst | 20 × 17.5 × 15 | NED (24 months) |
| 33/F | Abdominal pain, swelling | Left flank | Cyst | ND | NED (10 months) |
| 33/F | Tiredness | Descending colon | Cyst | 15 × 13 × 9 | NED (12 months) |
| 48/F | Postprandial fullness | Ascending colon mesentery | Cyst | 15 × 13 × 9 | NED (8 months) |
| 41/F | Flank pain | Right upper quadrant | Cyst | 21 × 16 | NED (18 months) |
| 31/F | Abdominal distension | Right retroperitoneal space | Multilocular cyst | 21 × 16 × 10 | ND |
| 36/F | Abdominal distension | Right lower abdomen | Cyst | 12 × 8 | NED (6 months) |
| 39/M | Back pain | Left pararenal space | Cyst | 6.9 × 4.4 | NED |
| 56/F | Painful urination | Right kidney | Multilocular cyst | 28 × 22 × 8 | Recur (6 months later) |
| 45/F | Abdominal pain | Left lower abdomen | Cyst with nodule | 15 | NED (12 months) |
| 25/F | Kidney mass | ND | Cyst with papillae | 15 | NED (148 months) |
| 43/F | Pelvic pain | ND | Cyst with papillae | 14 | NED (1 months) |
| 48/F | Enlarged mass | ND | Multilocular cyst | 7 | NED (34 months) |
| 37/M | Abdominal pain, mass | Right abdomen | Multilocular cyst | 22 × 11 | NED (12 months) |
| 26/F | Abdominal distension, pain | Left lower quadrant | Cyst | 13 × 10 × 8 | ND |
| 65/F | Mass | ND | Septate cyst | ND | NED (6 months) |
| 23/F | Mass | ND | Cyst | ND | ND |
| 68/F | Palpable abdominal mass | Left kidney | Multilocular cyst | 15 × 11 × 9 | NED (12 months) |
| 56/F (this) | Incidental on radiology | Retroperitoneum | Unilocular cyst | 8 × 5 | NED (24 months) |
ND, not described; NED, no evidence of disease
| Age/Sex . | Symptom . | Location . | Imaging finding . | Size (cm) . | Outcome (months) . |
|---|---|---|---|---|---|
| 41/F | Abdominal pain and tumor | ND | ND | 12 × 10 × 9 | NED (ND) |
| 38/F | Abdominal pain and distension | Left lower abdomen | Multilocular cyst | 11 | Mediastinal node metastasis (48 months) |
| 47/F | LUQ mass | Left upper quadrant | ND | 13 | ND |
| 63/M | Abdominal pain | Right kidney | Cyst | 11 | ND |
| 62/F | Abdominal pain | Right flank | Hypodense mass | 12 × 8.5 | NED (18 months) |
| 68/M | Right abdominal mass | Right abdomen | Cyst | 16 × 14.5 × 10 | NED |
| 65/F | Abdominal distension | Left abdominal cavity | Multilocular cyst | 21 × 14 | NED (12 months) |
| 32/M | Incidental on radiology | Around vena cava | ND | 7 × 6 × 4.4 | ND |
| 44/M | Abdominal pain | Interaortocaval | Multiple retroperitoneal mass | Multiple (2–5) | NED (12 months) |
| 35/F | Pelvic pain | Rear of the cecum | Cyst | 28 | NED (24 months) |
| 22/F | Abdominal pain | Superior of uterus | Cyst | 20 × 17.5 × 15 | NED (24 months) |
| 33/F | Abdominal pain, swelling | Left flank | Cyst | ND | NED (10 months) |
| 33/F | Tiredness | Descending colon | Cyst | 15 × 13 × 9 | NED (12 months) |
| 48/F | Postprandial fullness | Ascending colon mesentery | Cyst | 15 × 13 × 9 | NED (8 months) |
| 41/F | Flank pain | Right upper quadrant | Cyst | 21 × 16 | NED (18 months) |
| 31/F | Abdominal distension | Right retroperitoneal space | Multilocular cyst | 21 × 16 × 10 | ND |
| 36/F | Abdominal distension | Right lower abdomen | Cyst | 12 × 8 | NED (6 months) |
| 39/M | Back pain | Left pararenal space | Cyst | 6.9 × 4.4 | NED |
| 56/F | Painful urination | Right kidney | Multilocular cyst | 28 × 22 × 8 | Recur (6 months later) |
| 45/F | Abdominal pain | Left lower abdomen | Cyst with nodule | 15 | NED (12 months) |
| 25/F | Kidney mass | ND | Cyst with papillae | 15 | NED (148 months) |
| 43/F | Pelvic pain | ND | Cyst with papillae | 14 | NED (1 months) |
| 48/F | Enlarged mass | ND | Multilocular cyst | 7 | NED (34 months) |
| 37/M | Abdominal pain, mass | Right abdomen | Multilocular cyst | 22 × 11 | NED (12 months) |
| 26/F | Abdominal distension, pain | Left lower quadrant | Cyst | 13 × 10 × 8 | ND |
| 65/F | Mass | ND | Septate cyst | ND | NED (6 months) |
| 23/F | Mass | ND | Cyst | ND | ND |
| 68/F | Palpable abdominal mass | Left kidney | Multilocular cyst | 15 × 11 × 9 | NED (12 months) |
| 56/F (this) | Incidental on radiology | Retroperitoneum | Unilocular cyst | 8 × 5 | NED (24 months) |
| Age/Sex . | Symptom . | Location . | Imaging finding . | Size (cm) . | Outcome (months) . |
|---|---|---|---|---|---|
| 41/F | Abdominal pain and tumor | ND | ND | 12 × 10 × 9 | NED (ND) |
| 38/F | Abdominal pain and distension | Left lower abdomen | Multilocular cyst | 11 | Mediastinal node metastasis (48 months) |
| 47/F | LUQ mass | Left upper quadrant | ND | 13 | ND |
| 63/M | Abdominal pain | Right kidney | Cyst | 11 | ND |
| 62/F | Abdominal pain | Right flank | Hypodense mass | 12 × 8.5 | NED (18 months) |
| 68/M | Right abdominal mass | Right abdomen | Cyst | 16 × 14.5 × 10 | NED |
| 65/F | Abdominal distension | Left abdominal cavity | Multilocular cyst | 21 × 14 | NED (12 months) |
| 32/M | Incidental on radiology | Around vena cava | ND | 7 × 6 × 4.4 | ND |
| 44/M | Abdominal pain | Interaortocaval | Multiple retroperitoneal mass | Multiple (2–5) | NED (12 months) |
| 35/F | Pelvic pain | Rear of the cecum | Cyst | 28 | NED (24 months) |
| 22/F | Abdominal pain | Superior of uterus | Cyst | 20 × 17.5 × 15 | NED (24 months) |
| 33/F | Abdominal pain, swelling | Left flank | Cyst | ND | NED (10 months) |
| 33/F | Tiredness | Descending colon | Cyst | 15 × 13 × 9 | NED (12 months) |
| 48/F | Postprandial fullness | Ascending colon mesentery | Cyst | 15 × 13 × 9 | NED (8 months) |
| 41/F | Flank pain | Right upper quadrant | Cyst | 21 × 16 | NED (18 months) |
| 31/F | Abdominal distension | Right retroperitoneal space | Multilocular cyst | 21 × 16 × 10 | ND |
| 36/F | Abdominal distension | Right lower abdomen | Cyst | 12 × 8 | NED (6 months) |
| 39/M | Back pain | Left pararenal space | Cyst | 6.9 × 4.4 | NED |
| 56/F | Painful urination | Right kidney | Multilocular cyst | 28 × 22 × 8 | Recur (6 months later) |
| 45/F | Abdominal pain | Left lower abdomen | Cyst with nodule | 15 | NED (12 months) |
| 25/F | Kidney mass | ND | Cyst with papillae | 15 | NED (148 months) |
| 43/F | Pelvic pain | ND | Cyst with papillae | 14 | NED (1 months) |
| 48/F | Enlarged mass | ND | Multilocular cyst | 7 | NED (34 months) |
| 37/M | Abdominal pain, mass | Right abdomen | Multilocular cyst | 22 × 11 | NED (12 months) |
| 26/F | Abdominal distension, pain | Left lower quadrant | Cyst | 13 × 10 × 8 | ND |
| 65/F | Mass | ND | Septate cyst | ND | NED (6 months) |
| 23/F | Mass | ND | Cyst | ND | ND |
| 68/F | Palpable abdominal mass | Left kidney | Multilocular cyst | 15 × 11 × 9 | NED (12 months) |
| 56/F (this) | Incidental on radiology | Retroperitoneum | Unilocular cyst | 8 × 5 | NED (24 months) |
ND, not described; NED, no evidence of disease
In conclusion, although PRMCTB is rare entity, we need to be aware of this borderline tumor, as it can transform into mucinous cystadenocarcinoma, and early detection is crucial for appropriate treatment.
Conflict of interest statement
None declared.
Funding
None declared.
Ethical approval
The study was approved by the ethics committee of Yeungnam University College of Medicine. The patient consent waiver was approved by the Institutional Review Board (IRB).



