-
PDF
- Split View
-
Views
-
Cite
Cite
Steven L Zhang, Sofeah Samsuddin, Lee Chee Meng, Sabrina Ngaserin, Allen Wei-Jiat Wong, Abdominal-based free flap reconstruction of the breast in a patient with prior cryolipolysis: a case report and literature review, Journal of Surgical Case Reports, Volume 2025, Issue 5, May 2025, rjae511, https://doi.org/10.1093/jscr/rjae511
Close - Share Icon Share
Abstract
Abdominal-based flaps, including deep inferior epigastric artery perforator and transverse rectus abdominis myocutaneous flaps, are workhorse flaps for autologous breast reconstruction. These flaps are vascularized by perforators originating from the deep inferior epigastric vessels and traversing through the rectus abdominis muscle and subcutaneous tissue to supply the skin. As such, previous abdominal procedures, such as liposuction, may compromise flap perfusion and affect the choice of reconstruction. While there are numerous studies investigating the impact of liposuction on abdominal-based flaps, there is limited data on the implications of cryolipolysis, which is a relatively newer modality of non-invasive body contouring that is gaining increasing popularity. We describe a case of autologous breast reconstruction in a patient who had undergone cryolipolysis, where a free transverse rectus abdominis myocutaneous flap was used as the perforators were too small for reliable perfusion of a deep inferior epigastric artery perforator flap.
Introduction
Breast cancer is a leading cause of cancer among women globally [1]. Breast reconstruction following mastectomy is becoming more common due to increasing awareness of its psychosocial benefits and availability of plastic surgery services [2]. Abdominal-based flaps, including deep inferior epigastric artery perforator (DIEP) and transverse rectus abdominis myocutaneous (TRAM) flaps, are workhorse flaps for autologous breast reconstruction and are vascularized by perforators originating from the deep inferior epigastric vessels and traversing through the rectus abdominis muscle and subcutaneous tissue to supply the skin. As such, previous abdominal procedures, such as liposuction, may compromise flap perfusion and increase the risk of complications, such as flap loss and fat necrosis, and are considered by many to be a relative contraindication to the use of a free DIEP flap [3–5].
As compared to liposuction, cryolipolysis is a non-invasive modality for localized fat reduction and body contouring, which is gaining increasing popularity in recent years [6]. It is based on the concept of controlled cooling or ‘cold panniculitis’, which leads to selective apoptosis of adipocytes, theoretically without damaging surrounding tissues and overlying skin [6, 7]. In clinical practice, however, severe frostbites and cold burns have been reported, likely attributed to vasoconstriction, tissue hypoxia, and thrombosis [6, 7]. While there are numerous studies investigating the impact of liposuction on abdominal-based flaps, there is limited data on the similar implications of cryolipolysis [2].
We describe a case of autologous breast reconstruction in a patient who had undergone cryolipolysis, where a free TRAM flap was used as the perforators were too small for reliable perfusion of a DIEP flap.
Case report
A 53-year-old female patient with right breast cancer was referred to the Plastic Surgery service for breast reconstruction. She had a past medical history of ankylosing spondylitis, which was well controlled with non-steroidal anti-inflammatory drugs and sulfasalazine. She had undergone one session of cryolipolysis (CoolScupting treatment) 2 weeks prior to the consult. There was no history of previous abdominal surgery.
On pre-operative evaluation, the patient had ecchymoses of bilateral flanks, which was attributed to cryolipolysis. Breast reconstruction options were discussed, and she was keen for autologous reconstruction with a free DIEP flap. She was counseled regarding the risks of flap failure and possible conversion to a free TRAM flap. Surgery was scheduled at a date 2 months after her cryolipolysis treatment.
Computed tomography angiography (CTA) of the abdomen was performed, which demonstrated three perforators on each side, with a maximum diameter of 1 mm (Fig. 1). The perforator locations were marked following corroboration with bedside doppler ultrasound (Fig. 2).
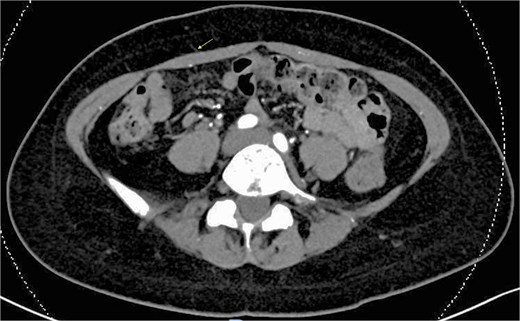
Preoperative CT angiography showing small maximum perforator diameter of 1 mm (arrow).

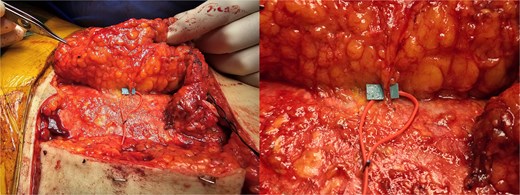
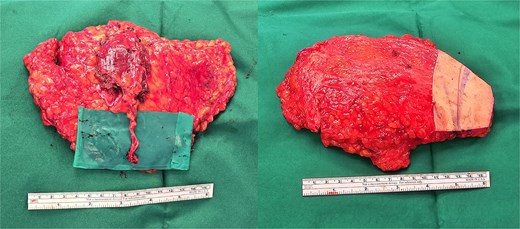
Reconstruction proceeded following nipple-sparing mastectomy by the breast surgeon (Fig. 3). The abdominal flap was divided in the midline, and the right side was chosen as the donor site for the free flap as it had the largest perforator on CTA. Exploration confirmed that the largest perforator was 1 mm in diameter (Fig. 4), which was deemed to be insufficient for reliable perfusion of a free DIEP flap. Hence, a muscle-sparing TRAM flap was used instead, incorporating the segment of muscle between the lateral and medial row perforators to maximize flap perfusion (Fig. 5). Flap perfusion was checked to be adequate prior to pedicle ligation. Microvascular anastomosis was performed on the internal mammary artery and veins with ethilon 9/0 sutures. Flap inset was completed, and the donor site was repaired with a prolene mesh and closed in layers over suction drains.

Postoperatively, the patient was monitored in the general ward. Flap monitoring was performed using clinical assessment and near-infrared spectroscopy (NIRS) [8]. Intermittent fluctuations of NIRS readings were noted during the first 2 days, which were attributed to likely vasospasm. The flap remained stable on subsequent monitoring, and the patient was discharged on postoperative day eight with no complications.
Discussion
Previous studies investigating the effect of liposuction on perforators have demonstrated a decrease in both perforator size and number on doppler ultrasonography following liposuction [4, 9, 10]. In a prospective study of six patients, Salgarello et al. [9] reported a decrease in the diameter of the two largest abdominal wall perforators of each patient following liposuction, from 1.0 to 3.3 mm preliposuction, to 1.0–1.8 mm postliposuction. In contrast, the largest perforator in our patient was 1 mm in diameter, both on preoperative CTA as well as direct visualization intraoperatively. This unusually small size is possibly due to prior cryolipolysis. Further studies measuring the perforator size before and after cryolipolysis would be useful to confirm our hypothesis.
To our understanding, there have only been two case reports of breast reconstruction using abdominal-based free flaps in the setting of prior cryolipolysis [2, 11]. Hyland et al. reported successful reconstruction with a free DIEP flap in a patient who had undergone cryolipolysis 5 years prior to surgery, where pre-operative CTA showed 6–7 viable perforators with no abnormalities [2]. Kankam et al. [11] reported successful reconstruction with a muscle-sparing TRAM flap in a patient who had undergone cryolipolysis <1 year prior to surgery, with no vessel abnormalities on preoperative CTA. In contrast, our patient had abnormally small perforator sizes. This could be related to a shorter time interval from cryolipolysis to surgery (2 months), although this is difficult to interpret given limited patient numbers.
The factors affecting the decision to convert from a DIEP flap to a free TRAM flap vary between surgeons. Nahabedian et al. [12] reported that reconstruction with a DIEP flap is usually possible after identification of 1–2 perforators with a minimum diameter of 1.5 mm. We find this to be a reliable guide, as perforators smaller than 1.5 mm in size are unlikely to provide reliable perfusion for the entire flap. In such cases, a free TRAM flap would be more reliable.
In conclusion, this case highlights potential challenges of performing autologous breast reconstruction using abdominal-based flaps in the setting of prior cryolipolysis. Careful preoperative assessment and counseling is important, ideally with CTA to evaluate for perforator course and size. If the perforators are not suitable for a DIEP flap, the free TRAM flap is a useful backup option.
Conflict of interest statement
None declared.
Funding
None declared.
References
Author notes
Steven L. Zhang and Sofeah Samsuddin are co-first authors and contributed equally to the writing of this paper.



