-
PDF
- Split View
-
Views
-
Cite
Cite
Ahmad Fasfoos, Obada Amro, Safaa Heeh, Walaa Zighan, Ansam Manasrah, Safa Bakri, Radwan Abu Karsh, Mahran Abu Sirrieh, Multidisciplinary management of a neonate with oropharyngeal teratoma and bilateral cleft lip and palate: a rare congenital presentation, Journal of Surgical Case Reports, Volume 2025, Issue 5, May 2025, rjaf293, https://doi.org/10.1093/jscr/rjaf293
Close - Share Icon Share
Abstract
This case report describes a rare presentation of a male infant with a large congenital oropharyngeal teratoma, bilateral cleft lip and palate, and a low-type imperforate anus. The infant experienced airway obstruction at birth, necessitating immediate neonatal intensive care unit admission and surgical intervention. Imaging revealed craniofacial teratoma involvement, contributing to palatal fusion failure during embryonic development. Two major surgeries were performed: teratoma excision and anoplasty. Postoperatively, the infant faced respiratory distress, Klebsiella sepsis, and a urinary tract infection, all successfully managed. The coexistence of craniofacial teratoma with bilateral cleft lip and palate is exceptionally uncommon, highlighting the need for early diagnosis, multidisciplinary collaboration, and meticulous surgical planning to ensure optimal outcomes.
Introduction
Teratomas are the most common extragonadal germ-cell tumors of childhood from pluripotent cells [1, 2]. Craniofacial teratomas are rare, comprising <10% of cases [3]. These tumors can be benign or malignant, with malignant forms often aggressive and locally invasive [4, 5].
Cleft palate results from incomplete fusion of the palatal shelves, while cleft lip arises from failed fusion of the maxillary and medial nasal prominences. Teratomas from the nasal septum may disrupt palatal fusion during development [6]. The coexistence of teratoma with cleft lip and palate is uncommon [7].
This report describes a male infant with large congenital oropharyngeal teratoma causing airway obstruction and bilateral cleft lip and palate, with a necessitated a multidisciplinary approach.
Case presentation
A male infant was delivered via cesarean section at 38 weeks of gestation due to breech presentation, with a birth weight of 2900 g. The baby was born vigorous, with Apgar scores of 7 at 1 minute and 9 at 5 minutes. At birth, a bilateral cleft lip and palate were observed, along with a large swelling protruding from the oropharynx that compromised his airway (Fig. 1). He was immediately transferred to the neonatal intensive care unit (NICU) for specialized care.

Clinical appearance of preoperatively large oropharyngeal swelling associated with a cleft palate.
Upon NICU admission, the infant developed respiratory distress with oxygen desaturation, requiring oxygen therapy. Respiratory acidosis was detected in the initial blood gas but improved with intervention. However, recurrent distress required multiple intubations. Imaging revealed possible atelectasis in the left lower lobe. Cardiovascular evaluation showed no abnormalities, but echocardiography identified an atrial septal defect (ASD), a patent foramen ovale (PFO), and a small patent ductus arteriosus (PDA). Ventricular function remained good.
The mother’s pregnancy was uneventful, with no significant complications. Both parents are consanguineous, with five healthy siblings and no family history of congenital anomalies. Neurological examination indicated normal reflexes and responsiveness, with transient postoperative hypotonicity resolving within a day.
Gastrointestinal evaluation revealed a low-type imperforate anus (Fig. 2) and anoplasty was performed on Day 7. The infant remained NPO, receiving total parenteral nutrition during this period. Renal function was normal, with a normal renal ultrasound ruling out VACTERL syndrome (vertebral defects, anal atresia, cardiac defects, tracheo-esophageal fistula, renal anomalies, and limb abnormalities). Hematological tests showed normal counts except for postoperative anemia requiring transfusion.

The infant underwent two major surgical interventions. The first was the enucleation of a large congenital oropharyngeal teratoma, performed four days after birth. The teratoma consisted of two palatal masses: one extending from the vomer mucosa to the extraoral region, and the other from the alveolar ridge to the soft palate (Fig. 3). Histopathology confirmed the diagnosis of a congenital oropharyngeal teratoma (Fig. 4). The second procedure was an anoplasty for the imperforate anus.
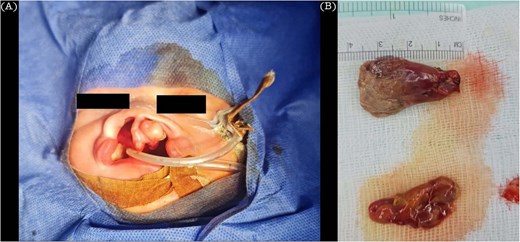
(A) Clinical appearance of pateint teratoma removal. (B) Two soft mass after removal the biggest measuring 2.3 × 1.5 × 1.2 cm in greatest dimensions.
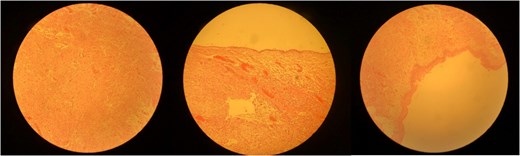
The cyst is lined by squamous epithelial cells without atypia. In the wall there are variable amount of different elements including upper respiratory type mucus secreting epithelium, glial tissue and small focus of granulomatous reaction.
After 25 days in the NICU, the infant was discharged. Follow-up after 6 month was patient in good health.
Discussion
In newborns, teratomas, especially those positioned in the craniofacial aspects, are considered to be extremely uncommon, accounting for <10% of all extragonadal germ-cell cancers. These tumors, which frequently develop from pluripotent cells [1, 8], contain a wide spectrum of malignancy, with the malignant varieties demonstrating invaded growth and the ability to spread [4, 5]. Facial teratomas are difficult to treat and manage, especially when they occur along with associated conditions such as bilateral cleft lip and palate, which is present in this circumstance [9]. Cleft lip and palate occur bilaterally for a number of reasons that are genetic and environmental [10, 11]. In addition, it is uncommon to see a case of a bilateral cleft lip and palate accompanied by a teratoma, thus this case is very special.
The earlier review articles on craniofacial teratomas of neonates have addressed on the difficulties in airway management and surgical treatment of the condition which usually require team effort [9, 12]. In this instance, because of the bilateral clefts, teratoma and other associated structures more careful surgical planning was paramount to avoid the complications of airway obstruction as well as the challenges presented by the cleft structures.
Craniofacial teratomas with cleft lip/palate require imaging, histopathology, and teamwork with surgeons, neonatologists, and anesthetists. Early diagnosis is crucial due to potential airway obstruction [13]. In the NICU, stabilization involved oxygen support, blood gas monitoring, and repeated intubation due to persistent respiratory distress. Cardiovascular assessment showed ASD, PFO, and PDA, requiring monitoring but no activity restrictions. Additionally, the child had a low-type imperforate anus needing anoplasty. Studies noted associations with epignathus, highlighting the complexity of the condition [8].
This case highlights the importance of family history in congenital malformations. Despite normal parents, the first-degree relationship could take into consideration some hereditable factors in the infant’s complicated picture. Lack of antenatal scanning likely delayed early diagnosis and preparedness for potential complications.
In conclusion, this case is a rare and complex presentation of a male infant with bilateral cleft lip and palate and a large oropharyngeal teratoma that necessitated a multidisciplinary approach. Compared to isolated cases of teratoma or cleft lip and palate, the coexistence of both conditions increases the complexity of surgical and airway management. The case emphasizes the critical role of early detection, the need for specialized neonatal care, and a coordinated surgical plan to optimize outcomes.
Conflict of interest statement
The authors assert that no conflicts of interest exist in relation to this work.
Funding
None declared.
Data availability
The article contains all the data that support the study’s findings and are readily accessible.
Research ethics and patient consent
This case report did not undergo an Ethics Committee review. The patient’s mother provided consent for publishing this case and its accompanying images.



